Did you know that Remote Patient Monitoring reduced hospital readmission by 76%?
Well, the Center for Medicare and Medicaid Services (CMS), in order to reduce the overall healthcare cost, introduced the RPM program. This not only marked the transformation of healthcare practices from traditional to digital but also instilled value-based practices.
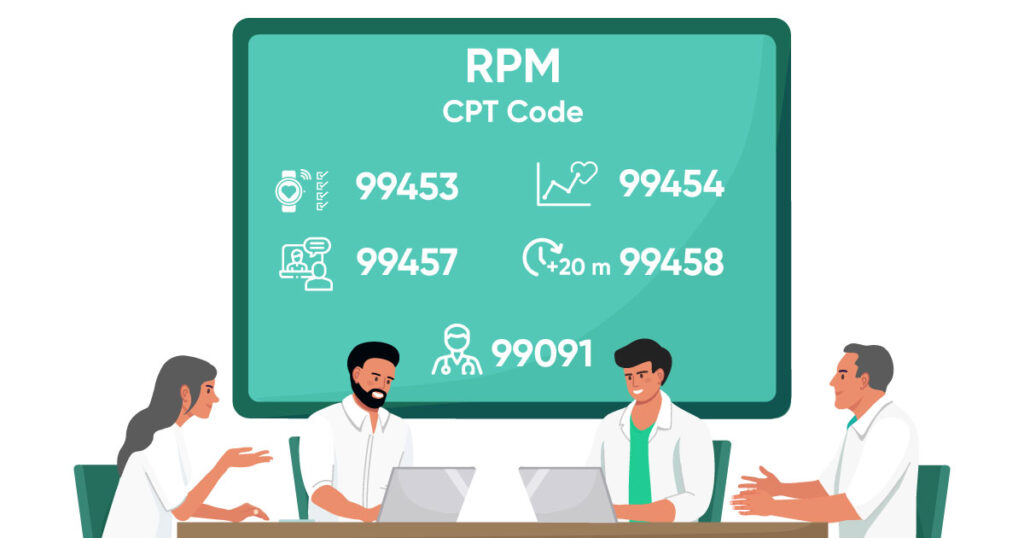
Understanding Eligible Services & Billing Codes
| RPM CPT Codes | Services Covered & Reimbursement Rates |
|---|---|
| CPT Code 99453 | Initial Set-up cost and patient education on using the RPM Devices. The national average for this CPT Code is $19.04. |
| CPT Code 99454 | Usually billed every month for the subsequent month of remote monitoring with collecting and transmission of data. The national average for this CPT Code is $55.72. |
| CPT Code 99457 | This CPT Code covers the initial 20 minutes of monitoring for patients after a face-to-face visit with the healthcare provider. The national average for this CPT Code is $50.18. |
| CPT Code 99458 | This is an additional code to CPT Code 99457 which covers the additional 20 to 40 minutes of monitoring of patient’s data. This code can be used twice in a month depending on the complexity of the situation. The national average for this CPT Code is $40.82. |
| CPT Code 99091 | This CPT Codes covers the services provided by physicians for monitoring the patient’s health and data for a minimum of 30 minutes. This code can be billed every month and the national average for this CPT code is $56.47. |
Download Free Checklist for all CMS Approved Remote Patient Monitoring Services
Download nowPatient Selection & Informed Consent
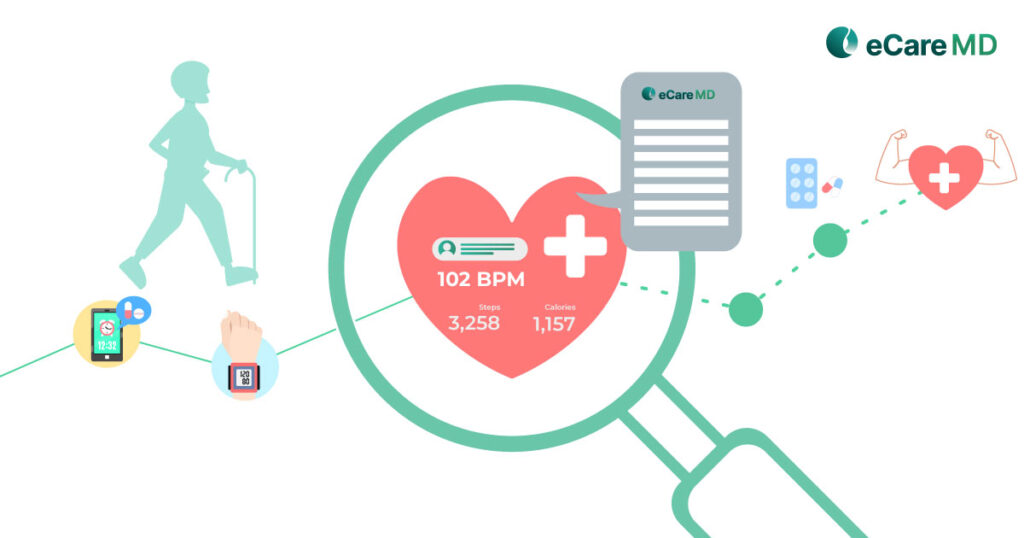
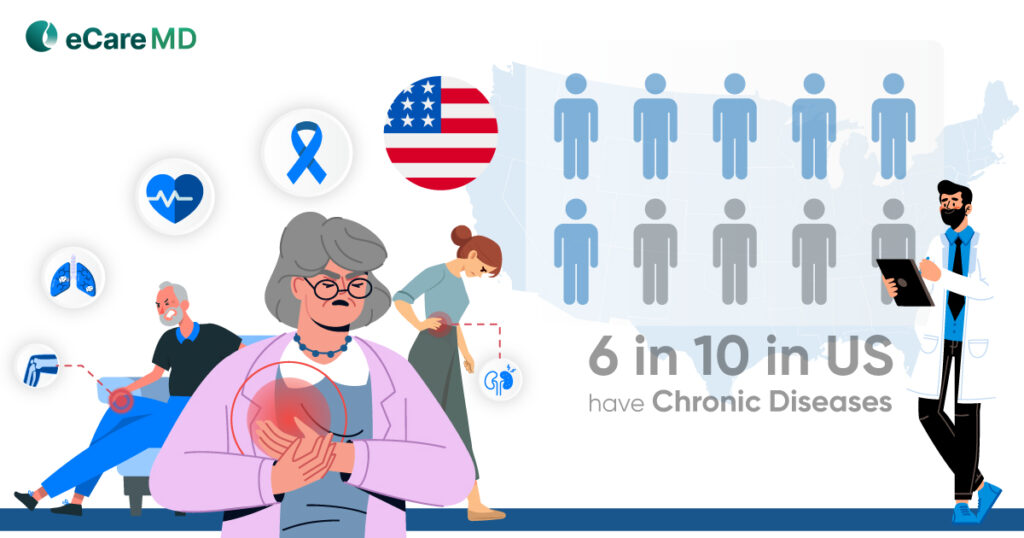
1. Chronic Condition: To enroll the patient under a remote patient monitoring program, the patient must have at least one documented chronic condition requiring medical diagnosis for at least six months. Along with that, the patient must also be at risk for serious complications to enable medicare coverage under the RPM program for better chronic disease management.
2. Medical Necessity: The monitoring requirements set by CMS for the RPM program require the patient to remotely monitor the physiological data to improve their health conditions and prevent complications with proactive preventive care.
3. Established Patient-Provider Relation: CMS requires a documented and established relationship between the patient and provider to enroll under the RPM program. This is enacted to ensure continuity of care and facilitate effective patient-provider communication with already established patient engagement in their healthcare activities.
4. Patient Suitability: Remote patient care heavily depends on the RPM software, devices, and the patient’s capability to use the technology to enable remote monitoring. CMS has recognized this and has listed some of the factors in its guidelines for enrolling patients in the RPM program. These patient suitability guidelines include access to necessary equipment, basic technical skills to operate monitoring devices and transmit data, and the patient’s mental capacity to understand and actively participate in the program.
5. Patient Consent: The most important aspect for patient selection other than all the four elements mentioned above is patient consent. Without patient consent one cannot enroll patients into the CMS RPM program and cannot even receive reimbursement for the services provided to them. The informed consent can be verbal or written from the patient indicating their wish to join the program and receive remote patient care.
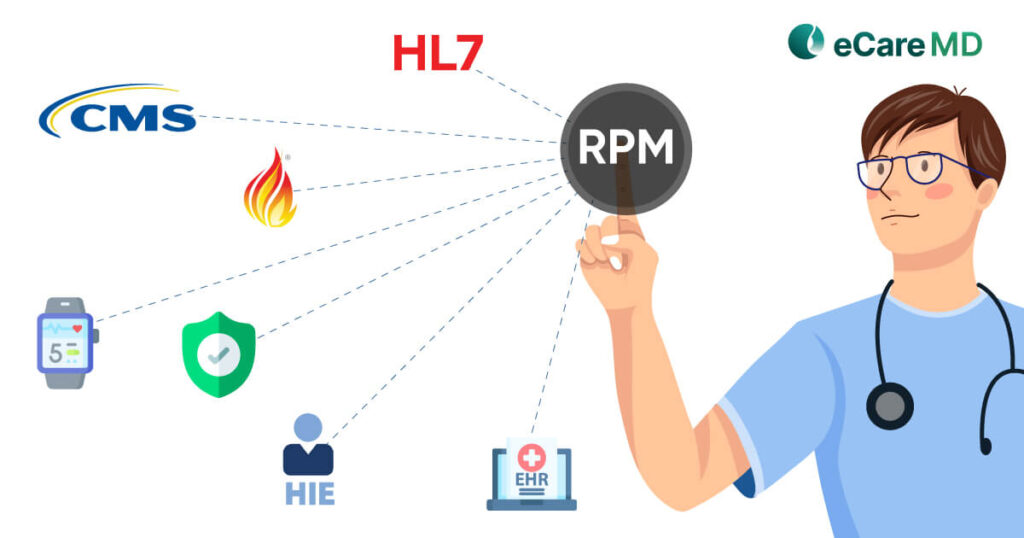
Technology Requirements & Data Security
1. CMS-Approved RPM Devices: Though CMS has not directly approved any specific RPM devices for the RPM program, CMS requires the RPM devices to be qualified or approved by FDA (Food and Drug Administration). Along with that, the device should be capable enough to automatically collect and transmit data to the provider’s system.
2. Permissible Devices: Some of the examples of permissible devices are:
- Blood Pressure Monitors
- Blood Glucose Monitors
- Pulse Oximeters
- Weight Scales, etc.
3. Data Security & Privacy Measures: Since the RPM programs deal with the collection and transmission of sensitive patient health information, it is necessary to safeguard their data and maintain telehealth platform security while remotely monitoring patients. Adhering to regulatory bodies like HIPAA, HITECH Act, etc., can not only help in ensuring data security in RPM programs but also avoid legal complications.
4. HIPAA Compliance: CMS has emphasized the importance of HIPAA compliance in protecting patient data. This is because of the strong guidelines that it has set for protecting patient data.
Coding, Billing & Reimbursement
1. Accurate Coding Practices: The CMS requires you to use the right CPT codes for the services provider under the RPM program. Since proper documentation is necessary for every code, incorrect coding can lead to reimbursement claim denials.
2. Documentation for Billing Claims: To support RPM claims that you are submitting to CMS, you need to document every service you provide to your patients. For example, detailed documentation of 20 minutes of care planning is required when using CPT Code 99457.
For detailed information about the RPM billing codes and guidelines, here is the link to the official website here.
Continuous Quality Improvement and Auditing
Conclusion
CMS is the reason why we are able to harness technology in healthcare services. It has not only reduced the burden and overall spending on healthcare services but also made receiving healthcare more convenient.
The best way to navigate through the CMS regulations for RPM is to adhere. Consider all the things that are necessary for the program and check for their compliance with the CMS. This will ensure that the success of the program is on track and that you will be paid rightly for the service you provide.
Being the regulatory and healthcare provider starting out the RPM program, you must be updated with the latest updates in CMS RPM regulations. This will make you proactive in ensuring compliance with the healthcare regulations and will allow you to make informed decisions.
Frequently Asked Question’s
- Eligible patients: Must be chronically ill and have a condition that can be monitored remotely.
- Patient consent and education: Patients must consent to remote monitoring and understand how their data will be used.
- Billing provider: A healthcare professional must order and oversee the remote monitoring.
- Data security: CMS requires HIPAA compliance to protect patient privacy and data security.
- Minimum data collection: At least 16 days of data collection per 30-day period is required for certain services.
- Established patient relationship (RPM only): For RPM services, a prior in-person visit is required, with some exceptions.
- Stay informed: Regularly review updates to CMS regulations and guidelines.
- Internal controls: Implement procedures to monitor and track compliance within your practice.
- Regular audits: Conduct internal audits to identify and address any gaps in compliance.
Here are some of the consequences of non-compliance with CMS regulations in RPM:
- Financial penalties: Non-compliance can result in significant fines levied by regulatory bodies.
- Data access restrictions: Regulatory bodies may restrict access to your data in order to investigate non-compliance.
These are just two of the potential consequences, and compliance is important to avoid these risks.
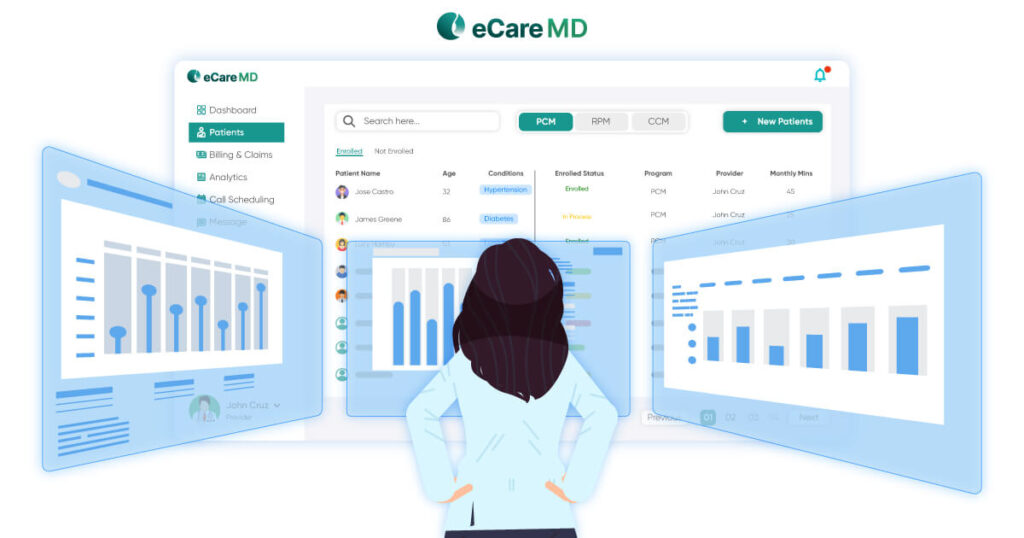
Technology plays a crucial role in facilitating compliance with CMS guidelines for RPM by:
- Enabling secure transmission of patient data between monitoring devices and healthcare providers.
- Streamlining data collection and storage through wearable sensors and mobile apps, reducing manual burden.
- Facilitating real-time monitoring and generating alerts for concerning vitals, ensuring timely intervention.
- Supporting remote care coordination by allowing providers to remotely review patient data and adjust treatment plans.