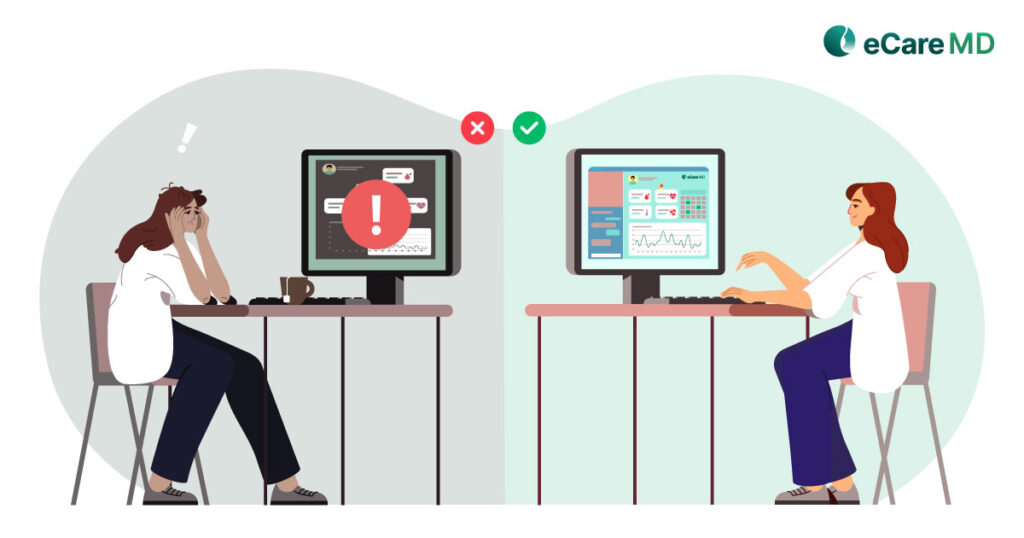
Nowadays, there are numerous problems facing healthcare professionals in coordination with patients while delivering care with fragmented patient records, communication channels and concerns with security and privacy. These parameters can lead to gaps in care and exchanging patient information, duplication of tests and treatments and delays in quality care transition directly impacting on patient outcome and negative satisfaction.
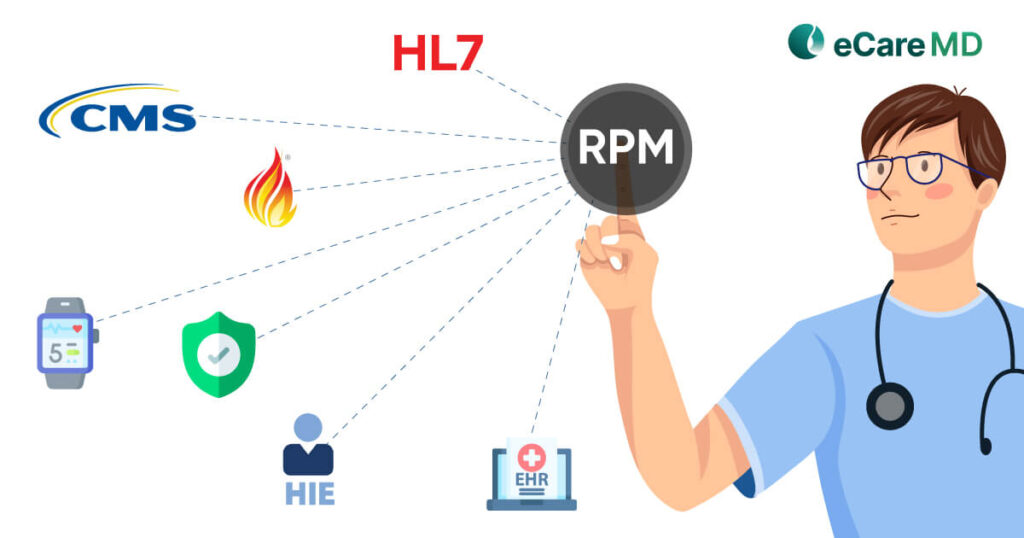
Furthermore,inadequate workflows of practices,care team collaboration and staff burnouts are major barriers to provide quality care coordination services to patients. To overcome those barriers there should be a requirement of establishing proper communication channels and protocols,multidisciplinary care team ,robust interoperability which can promote patient centered approaches in care delivery.
To improve patient outcome and quality of care delivered there is a need to establish proper communication and collaboration between healthcare providers and patients.Regular communication with patients can help providers to get involved and updated into patient healthcare journey which can enable providers to identify the future health risk or complexity. Efficient communication and collaboration are essential to ensure timely information sharing, reduce errors, and enhance patient outcomes.
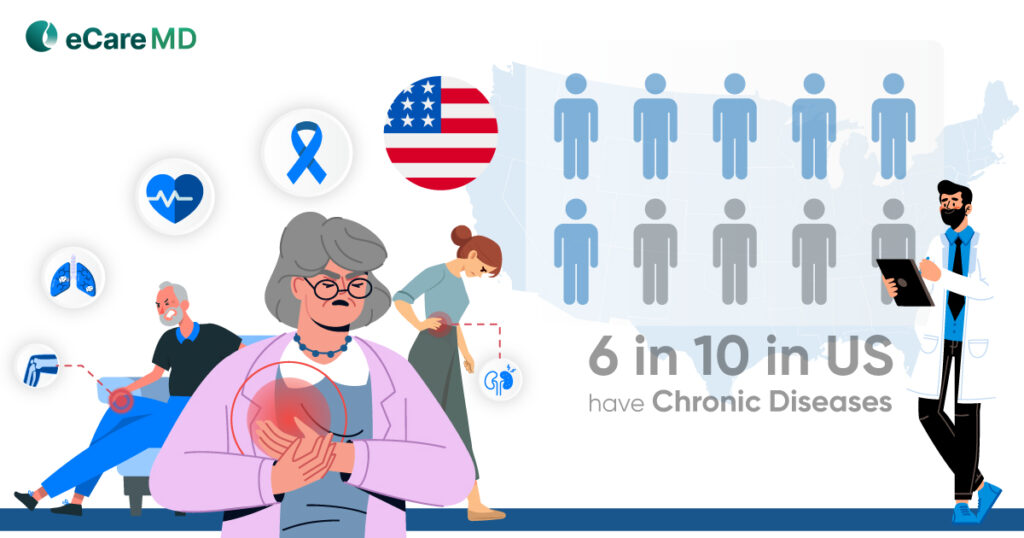
Additionally, with the increase in chronic diseases in the huge patient population, there is huge demand for continuous patient monitoring and working closely with patient health.To fulfill this need there is growing emphasis on holistic patient centered care coordination by improving communication and collaboration.Improved communication and collaboration facilitate care coordination, enable seamless transitions between care settings, and empower patients to be active participants in their care.
In traditional healthcare settings, there seems to be a lot of challenges to see patients and get their health updates regularly in between consecutive visits. Providers are not able to richout to patients due to an geographical barrier and lack of communication channels.Also healthcare professionals like doctors, nurse and specialists can not able to connect with patient to see health progress and facing difficulties in getting appropriate health updates due an inadequate communication channels.
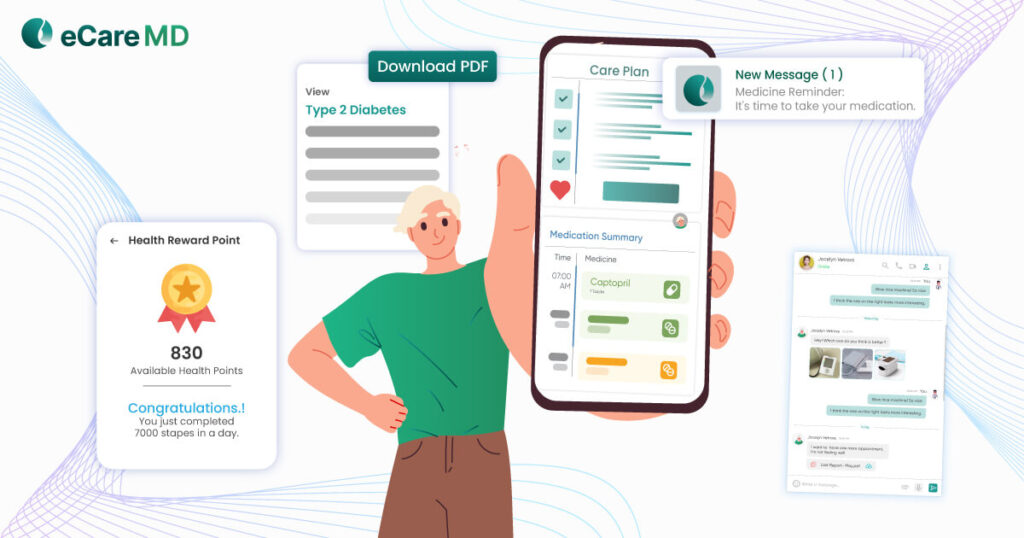
Implementing a good care coordination software, providers will be able to communicate with patients with various telehealth options such as audio /video calls, two way texting ,emails , scheduling ,patient information exchange, alert ,reminders and notifications.These all features allow healthcare providers to involve into an patient healthcare journey and encourage patients to take control of their own health.The advantage of communication done through care coordination platform is high secure ,encrypted and private so there is no any chance of patient health data breach.
Collaboration is another key aspect of any care coordination software which enables healthcare providers to communicate with each other to exchange information and get advice and take any necessary informed decisions for mutual patients to get them recovery quickly.Collaboration involves and task management, addressing patient need, consulting patient as and when required, providing necessary services and help patients to improve their health outcome.
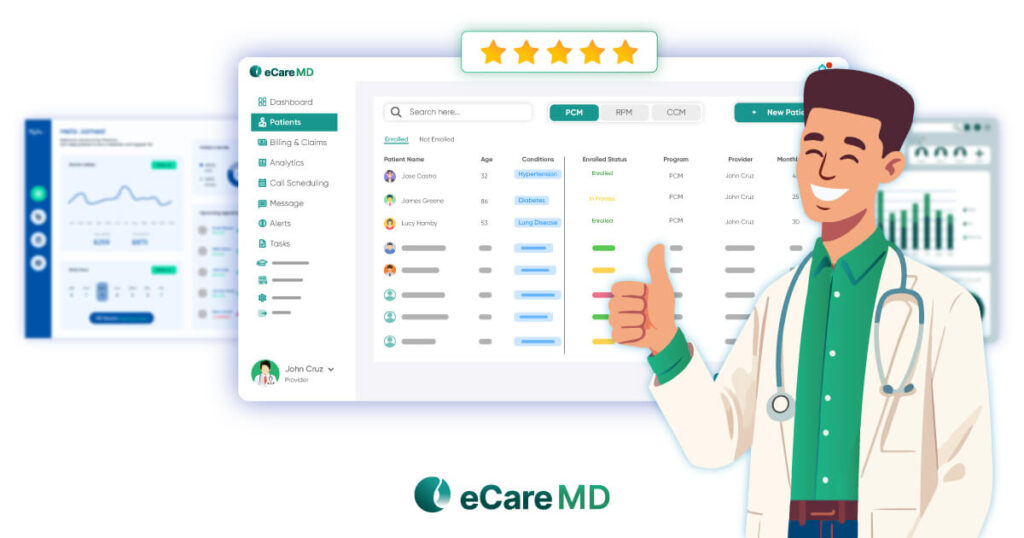
For better and improved patient outcomes , patients must follow the instructions provided by their care manager.But it is very difficult to encourage patients to follow given instructions by just calling them and giving orders.Also creating the care plans and maintaining it is a very big challenge while treating patients.Many of the patients having a multiple chronic conditions with higher risk so they need an complex care management.Complex care plan management is an crucial task and it can not possible to maintain by pen and paper or any other traditional healthcare platforms. Due to this , providers can not track patient progress from such care plans; they may lose the patients adherence to the treatment resulting in a lack of patient health outcome.
Care coordination software enables healthcare providers to create an electronic care plan by defining all measurable and non measurable goals , barriers including all patient medical records so that care managers track and document the progress.Also these care plans are stored electronically and can be shared securely to the patient and associated health care providers. Also these electronic care plans can be accessed securely through patient portal and mobile application.
Since electronic care plans are easy to access and accommodate, it improves the patient’s adherence towards care plans and encourages them to get their health into their control.Patients can add their vitals regularly, lab results,complete their tasks and document into the care plan progress so that providers can see the activities done in the care plan and take the necessary actions based on insights.
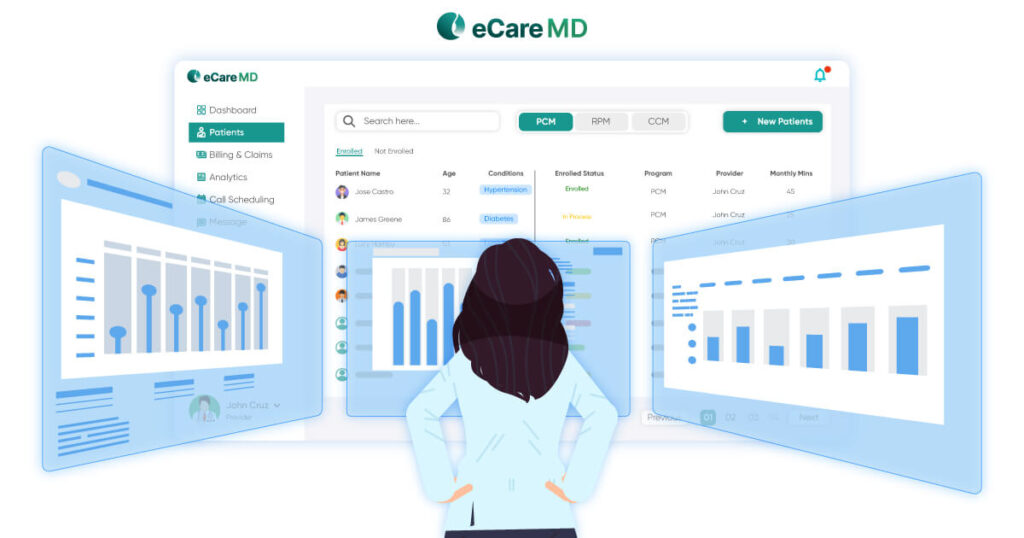
Using a simple EMR or healthcare platforms providers need to do manual and repetitive data entry which is a very time consuming and inefficient process where there might be a lot of chances of manual errors and duplicate treatment. Also, there has been difficulties to maintain and access those data securely with the platforms since it has limitations and difficult to navigating due to an complex workflows and lack of automations.
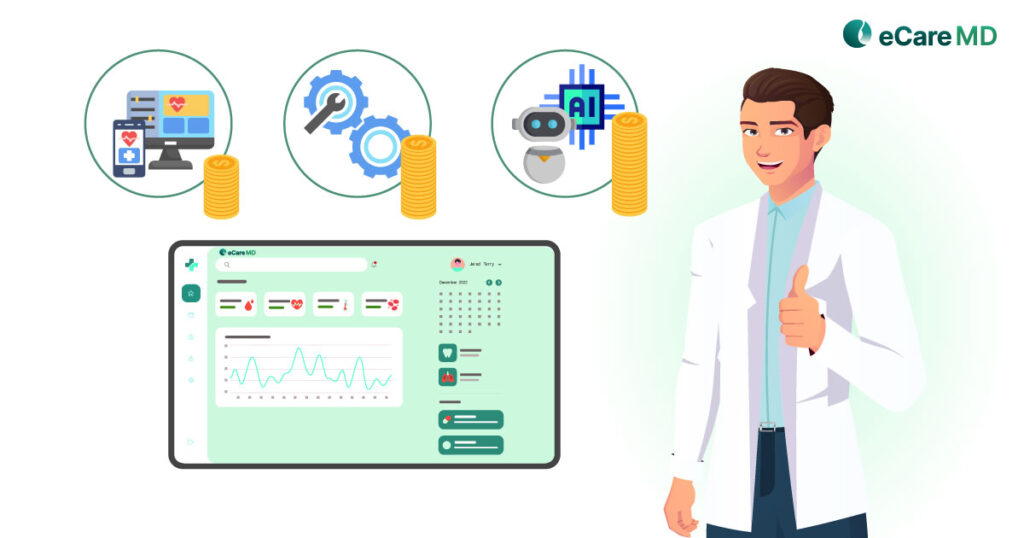
Care coordination software has a flexibility to customize each workflow and manage tasks for each provider efficiently.This feature streamline the administrative tasks and improve overall efficiency among the reducing staff burnout since it reduces the burden on every practitioner or practice user.
Care coordination software has well structured and mapped workflows for administrative tasks such as scheduling, appointment confirmations, sending of intake forms to patients, streamlines billing and claims process and insurance related tasks that can be done seamlessly.
Improved communication and care coordination in healthcare enhances patient engagement and satisfaction by creating a supportive environment. Clear communication and attentive listening empower patients and minimize confusion, while coordinated care ensures timely and comprehensive treatment. This fosters trust, leading to increased satisfaction and better health outcomes as patients feel valued and supported, encouraging active participation in their care and adherence to medical advice for improved well-being.
For better patient engagement and collaboration care coordination software has various communication channels such as two way calling, texting and emails.These features bridge the gap between patient and provider and make them coordinate with each other.In addition to that there are other features that can improve patient engagement like timely reminders, alerts and notification to make patient aware about their health updates.Furthermore task management is the best feature each care coordination software have which will make caregivers engaged and ensure every activity regarding patient should be done on time which ultimately improves the patient outcomes.
Additionally, the patient portal enables patients to access their medical records easily and encourages patients to communicate with their care team regularly.Timely reminders and alerts provide a health update and make patients aware and involve them into their own healthcare journey.
Leveraging healthcare data involves harnessing information from various sources such as patient records, clinical trials, and population health data to make informed decisions in healthcare. By analyzing this data, healthcare providers can identify patterns, trends, and insights to improve patient care, optimize resource allocation, and enhance overall healthcare delivery. This data-driven approach enables more precise diagnoses, personalized treatment plans, and proactive interventions, ultimately leading to better health outcomes for individuals and populations alike.
Care coordination software leverages the patient data in a structured and organized manner.Care coordination software generates reports and dashboards which gives insights about patient care transitions, progress, highlighting the areas of improvement, potential gaps in care and opportunities for improvement.These insights helps healthcare providers to predict any kind of risk associated with patient health,encourage to take an informed decision and preventive action to reduces future hospital readmissions and significant risk of patient death
The MIS reports can help practices to evaluate their performance throughout the year.It gives ideas to determine best practices to allocate resources more effectively, and make informed decisions to enhance practice efficiency, maintain the quality care and better patient outcome.