The rising cost of healthcare is a concern for everyone. While patients are struggling to meet the rising cost of care, providers are overburdened with traditional practices, which affects their practice’s efficiency. In a nutshell, accessing care has become a costly affair for almost everyone involved in the care delivery process.
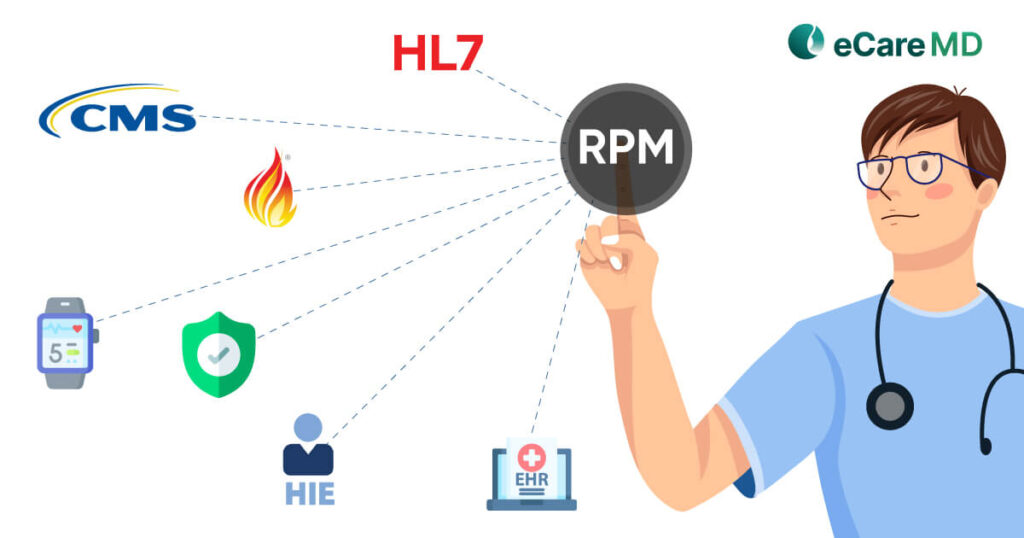
Today, Remote Patient Monitoring has become the first choice of consultation while receiving care services. Furthermore, RPM has successfully helped create a win-win situation in healthcare, and its inclusion in CMS programs like Medicare (Part A, B, C, and D), Medicaid, and CHIP (The Children’s Health Insurance Program) defined the roadmap for the future.
However, as a provider who will be investing significantly in building the Remote Patient Monitoring ecosystem, how would you increase revenue with RPM in CMS programs?
Well, let’s find out the financial benefits of RPM for chronic care management. Let this be the free guide to boosting ROI with RPM in CMS programs.
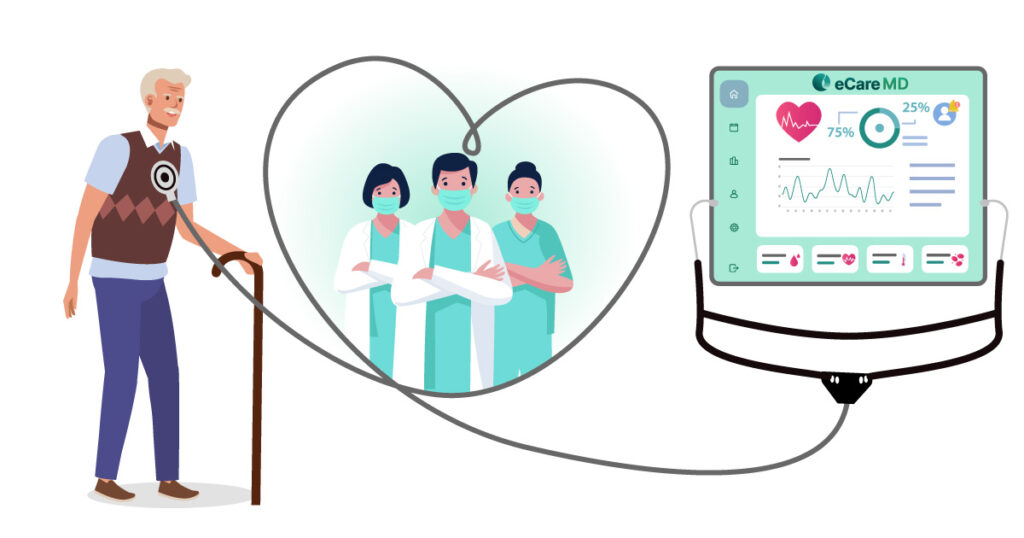
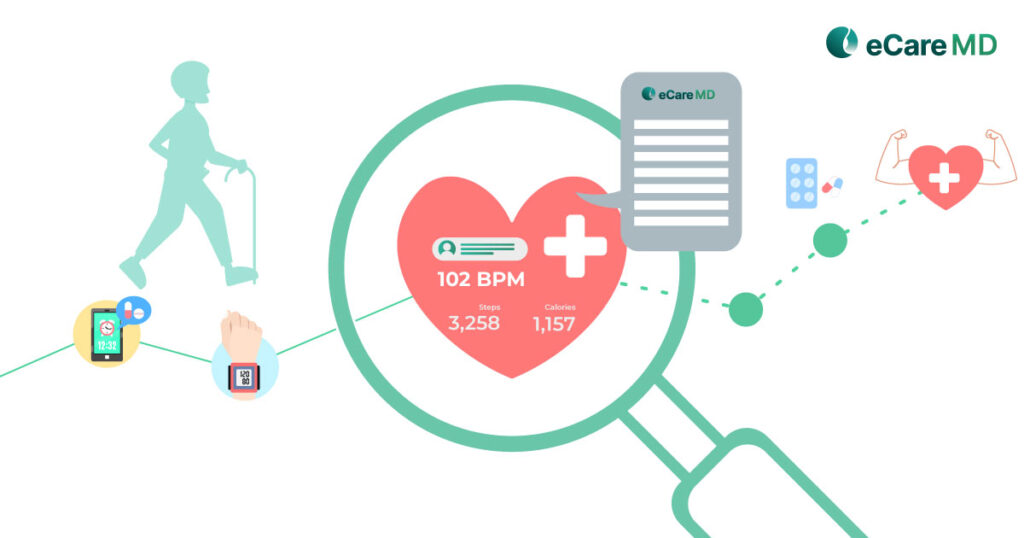
1. Early Detection & Interventions: Remote patient monitoring is majorly and effectively used for continuous monitoring of patients. Due to this, early detection of conditions becomes possible, and the real-time monitoring of patient’s health conditions allows providers to intervene, enabling better preventive care. This helps avoid any potential complications in health care and results in improved patient outcomes without the need to visit the hospital.
2. Proactive Care Management: By enabling early detection providers are a step ahead of the symptoms and timely intervention is made possible. By making accurate medication adjustments with remote consultation, the need for hospitalization is avoided, helping providers to better manage their physical resources and put them to optimum use.
3. Improved Patient Engagement: When patients are aware of their deteriorating condition, they tend to participate proactively in their care journey. This improves their engagement with the care services, leading to improved patient outcomes and faster results, helping to save significant healthcare expenditures for both providers and patients.
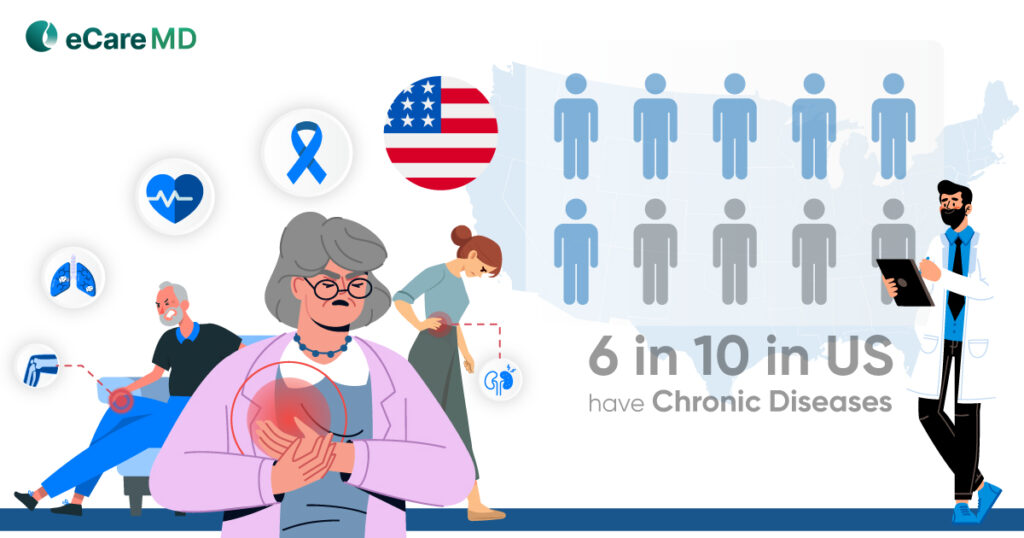
Another core aspect of healthcare where remote patient monitoring is used is in chronic care management. For effective chronic disease management using RPM, the cost-effectiveness of remote patient monitoring in ACOs (accountable care organizations) can be clearly seen. Let’s explore how:
1. Continuous Data Collection: Remote patient monitoring works in an ecosystem where every system is connected, forming a network that smoothly and securely allows the flow of healthcare data to enable virtual care. This data enables accountable care organizations to track the progress diseases have made and curate personalized care plans, which will result in improved patient outcomes.
2. Remote Monitoring & Adjustments: One of the best practices for implementing RPM for ROI maximization is to monitor medication adherence, vitals, and patient symptoms in a remote set-up. This way, the proper utilization of healthcare resources can be ensured, and it is one of the most effective ways of cost reduction in healthcare. The key to achieving this in healthcare has been the ability to make necessary adjustments in the care plan and inform the patient in real time to ensure they are updated with their care journey. This eliminates the need to visit the clinic for an in-person visit and better monitors patient health in real time.
3. Reduced Healthcare Costs: Increasing revenue with RPM in CMS programs comes in the form of saving by reducing the overall healthcare costs. For instance, the reduced hospital readmissions helps you to use the available resources optimally helping you to better manage chronic conditions and save significantly on the overall expenditure of healthcare by preventing complications and hospitalizations.
The Centers for Medicare and Medicaid Services (CMS) plays the role of a supporting partner in federal and state health insurance marketplaces. It helps in the implementation of the Affordable Care Act (ACA) to make healthcare affordable for everyone in the United States.
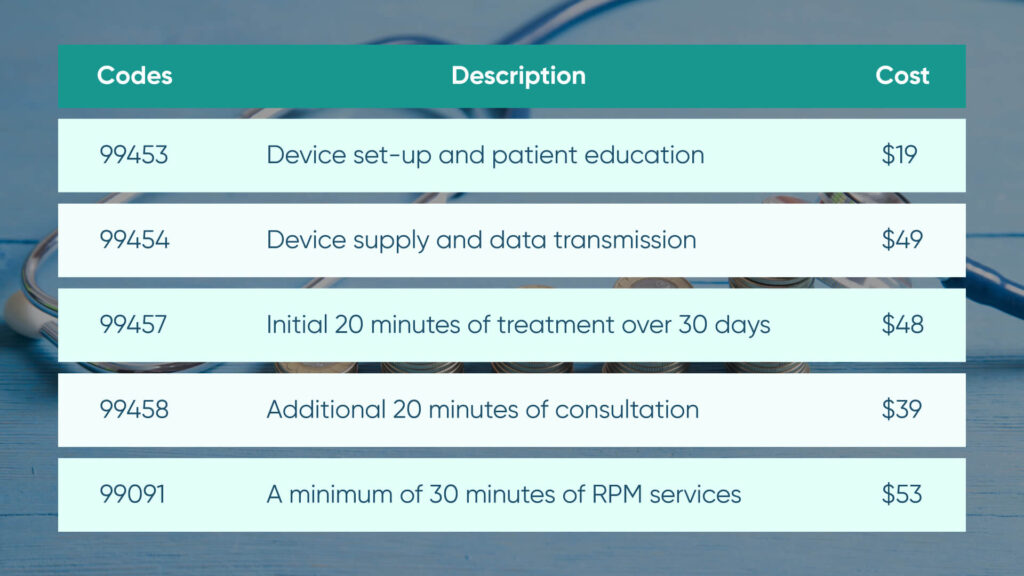
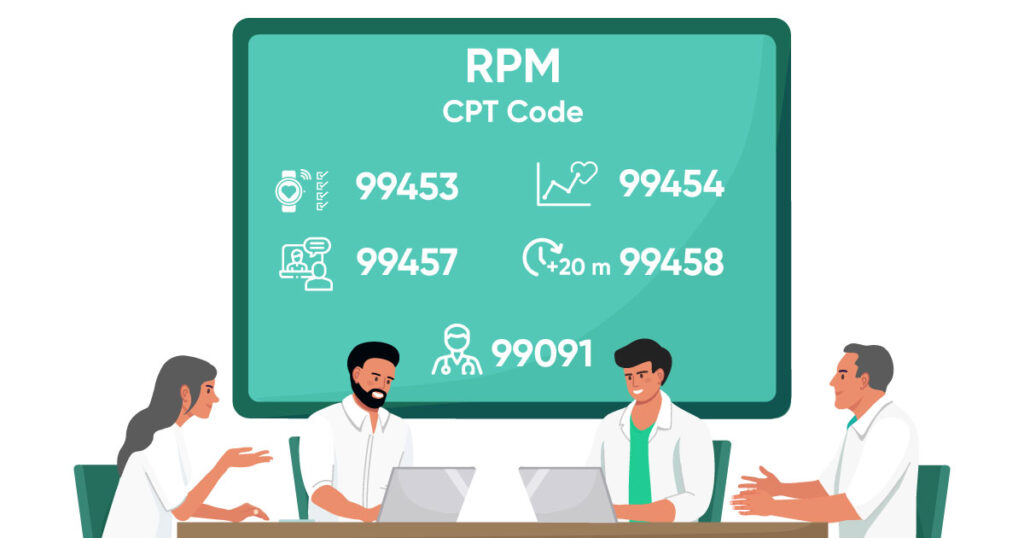
With regards to RPM reimbursement in your CMS program, CMS has released some of the CPT Codes for specific RPM services that you will provide. However, to maintain transparency and integrity in the care services, they have also implemented some provisions that make those CPT Codes valid.
One of the best practices for implementing RPM for ROI maximization is to streamline care coordination and communication between patients and providers. Let’s see how it contributes to maximizing your return on investment:
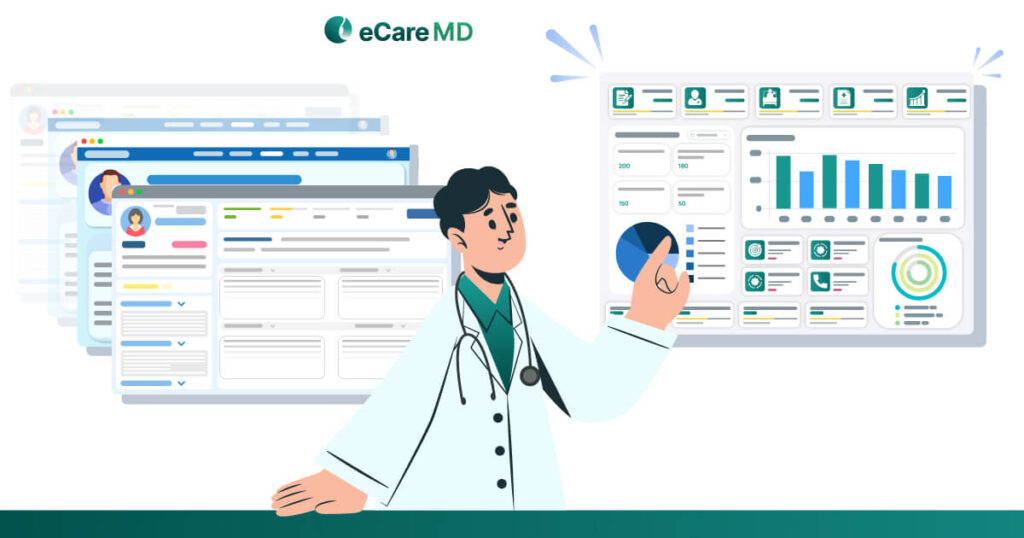
1. Improved Communication & Collaboration: Remote patient monitoring programs work in custom-created virtual ecosystems for delivery. For this, a virtual network of all the members involved in the patient’s care journey is connected, facilitating better communication and coordination between the care team and the patients. This allows the entire care team, involving patients, care providers, and specialists, to coordinate better and curate personalized care plans. With this, they also make sure that the appropriate care is given and that every member of the care team is working towards the same goal.
2. Real-time Data Sharing: The major advantage of remote patient monitoring is that despite being set up in a virtual ecosystem, it facilitates patient data sharing in real-time amongst different healthcare providers. This instills a more holistic approach while providing care where care is to the patient in real-time, and the nature of care delivery changes from reactive to proactive.
3. Increased Efficiency & Productivity: By improving the care coordination and communication it streamlines almost all the necessary communication channels in care delivery. Apart from that, the rest of the repetitive administrative tasks are streamlined by the remote patient monitoring software which greatly impacts the efficiency of the clinic, allowing care providers to focus more on patient care.
Did you know that almost 46% of millennials use remote patient monitoring, and with the aging population, the number is most likely to increase further? Following their footsteps, the upcoming generation (GenZ) is more likely to choose RPM services. By implementing RPM in your CMS program, you get a competitive advantage over other service providers.
Furthermore, the patient expectations of digital healthcare are evolving, and with innovations in RPM, you are most likely to meet them even before they become a mainstream trend in the healthcare industry. This can be your attractive USP to attract more patients.
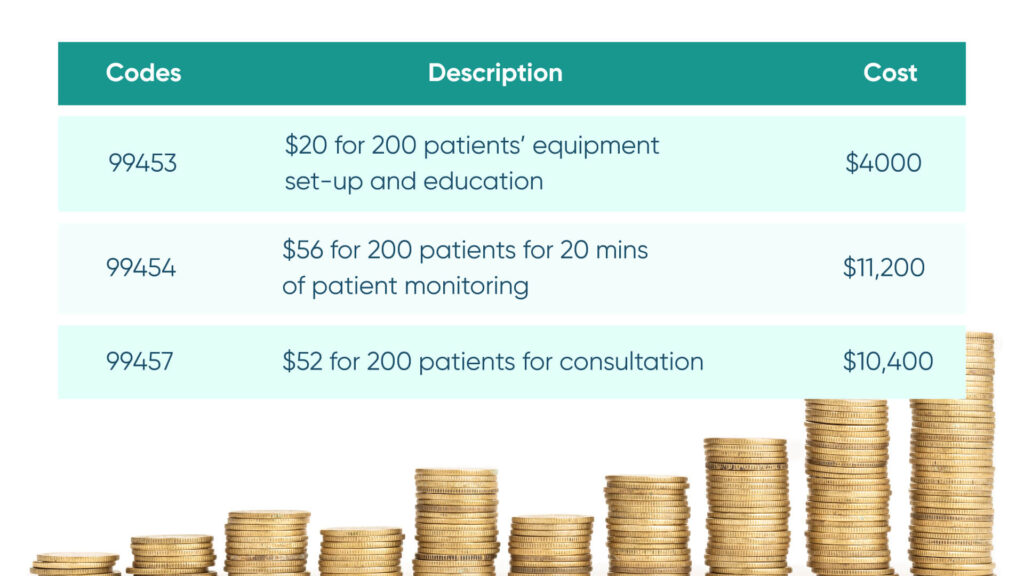
To give you an example of the return on investment for remote patient monitoring for your CMS program, let’s get our calculators out and get started.
So, suppose you are starting out your program, and the initial investment covering all the equipment, software, and developing infrastructure costs somewhere around $25,000. Now that the program has been initiated and you have enrolled around 200 patients in your program, here is the reimbursement you will most likely receive with these CPT codes.
So, the monthly reimbursement will stand at around $21600 and expand up to $263200 annually if all the patients enrolled in the program remain unchanged. However, some other consultation costs involve the salary of the care manager, which is somewhere around $40000 annually.
This means your ROI for the CMS RPM program would be $263200 – 40000 (care manager salary) – $25000 initial investment cost, which will be $198200.
However, one of the key performance indicators for financial success will directly reflect the care efficiency of your care practice. To further scale your practice and measure ROI over time, ensure you set realistic milestones and work towards achieving them.