Well, if you are dealing with the same problems and frustrated very much because of the unavailability of a proper care coordination platform, this blog is for you !
We will discuss step by step how to get started with care coordination services with the right software. Let’s discuss this.
Define Needs and Goals
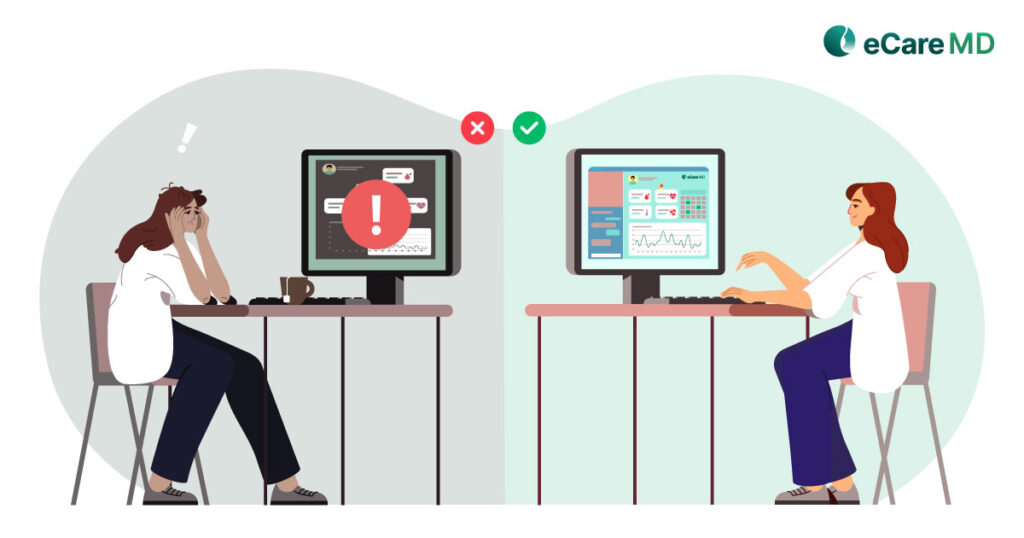
 To start with an implementation of care coordination software, healthcare providers must identify their requirements and end goals that need to be achieved from care coordination services. While defining the requirement, current practice workflows and operations needs to be taken into consideration. All pain points are making it difficult to provide quality care to the patients and directly affecting the practice performance.
To start with an implementation of care coordination software, healthcare providers must identify their requirements and end goals that need to be achieved from care coordination services. While defining the requirement, current practice workflows and operations needs to be taken into consideration. All pain points are making it difficult to provide quality care to the patients and directly affecting the practice performance.
Once these requirements and goals have been finalized, providers must check their compliance with regulatory requirements. For every healthcare software, HIPAA compliance must ensure that patient health information is secure and private without any data breach. Along with compliance, healthcare providers must check all regional regulatory requirements that are needed to deal with any healthcare software.
Research and Select Software
 There are a lot of companies in the market that provide healthcare software and care coordination software. It is very difficult to choose an appropriate software best suitable and fit for your requirements and goals. You can visit multiple healthcare technology companies’ websites and explore the softwares and their unique features that can fulfill your needs.
There are a lot of companies in the market that provide healthcare software and care coordination software. It is very difficult to choose an appropriate software best suitable and fit for your requirements and goals. You can visit multiple healthcare technology companies’ websites and explore the softwares and their unique features that can fulfill your needs.
While exploring the software that is best suited for your needs, you must explore and compare the features and functionalities that that software provides and the pricing for that as well. Many healthcare product companies are providing the packages for their software which basically varies based on the features and customization.
Assemble an Implementation Team
 After finalization of software, the next step towards the implementation is to identify the stakeholders that are actually going to use the software. These stakeholders includes personals from various departments and are internally associated with each step and process of the healthcare practices. Identify each stakeholders requirement and give them an idea about the software.
After finalization of software, the next step towards the implementation is to identify the stakeholders that are actually going to use the software. These stakeholders includes personals from various departments and are internally associated with each step and process of the healthcare practices. Identify each stakeholders requirement and give them an idea about the software.
Once the stakeholders have been identified, they must know their responsibilities and be appointed as project managers to drive the successful implementation of the project. The project manager consults with the stakeholders, transfers their feedback and requirements to the implementation team, and tries to get all requirements implemented as requested by the stakeholders. Also, the project managers can form a cross-functional team, including IT, clinical staff, and administrative personnel, to get things done at the right time and place. These team members take an active role in software implementation with respective departments since they are well aware of the operations and workflows.
Configuration and Training
 Each department of healthcare organization has different requirements for process and user accessibility. Some configuration is required to address those requirements. If the software does not have the capability to get ready as per configuration, then a gap between software functionalities and requirements is identified. To bridge that gap, customization might be required, which may be in the scope or out of the scope of the project, and there will be financial involvement.
Each department of healthcare organization has different requirements for process and user accessibility. Some configuration is required to address those requirements. If the software does not have the capability to get ready as per configuration, then a gap between software functionalities and requirements is identified. To bridge that gap, customization might be required, which may be in the scope or out of the scope of the project, and there will be financial involvement.
Data Migration and Go-Live
 Following configuration and training, there will be a data migration and go-live phase where the project manager needs to ensure all required master data and patient information aree new system, which, has to be implemented. To start with care coordination software in any healthcare organization, there should be patient information, including their clinical and contact information, and their insurance information needs to be migrated to treat patients efficiently.
Following configuration and training, there will be a data migration and go-live phase where the project manager needs to ensure all required master data and patient information aree new system, which, has to be implemented. To start with care coordination software in any healthcare organization, there should be patient information, including their clinical and contact information, and their insurance information needs to be migrated to treat patients efficiently.
Ongoing Support and Monitoring
 Once the software has been implemented successfully and all stakeholders in a healthcare organization start using it for routine activities, the project manager needs to monitor all activities and operations performed regarding care coordination to improve patient outcomes for the initial month. During this period, project managers need to plan for support for ongoing activities. Project managers can make a team of support people who can closely work with all users and resolve their issues on time. If any issue is not resolved, then the support team can do the troubleshooting and try to get those resolved with the help of a technical team from the software side.
Once the software has been implemented successfully and all stakeholders in a healthcare organization start using it for routine activities, the project manager needs to monitor all activities and operations performed regarding care coordination to improve patient outcomes for the initial month. During this period, project managers need to plan for support for ongoing activities. Project managers can make a team of support people who can closely work with all users and resolve their issues on time. If any issue is not resolved, then the support team can do the troubleshooting and try to get those resolved with the help of a technical team from the software side.
Conclusion
To start with, care coordination software has a long process, but it is well worth it and beneficial for better practice management to optimize efficiency and patient care. This article outlines steps for implementing care coordination software effectively. It emphasizes the importance of understanding needs and goals, ensuring compliance, and defining metrics for success. Researching and selecting suitable software involves exploring features, pricing, scalability, and interoperability. Assembling an implementation team, configuring the software, and providing thorough training are crucial. Data migration and a successful go-live phase precede ongoing support, monitoring, and adaptation to optimize system performance and user satisfaction.Frequently Asked Question’s
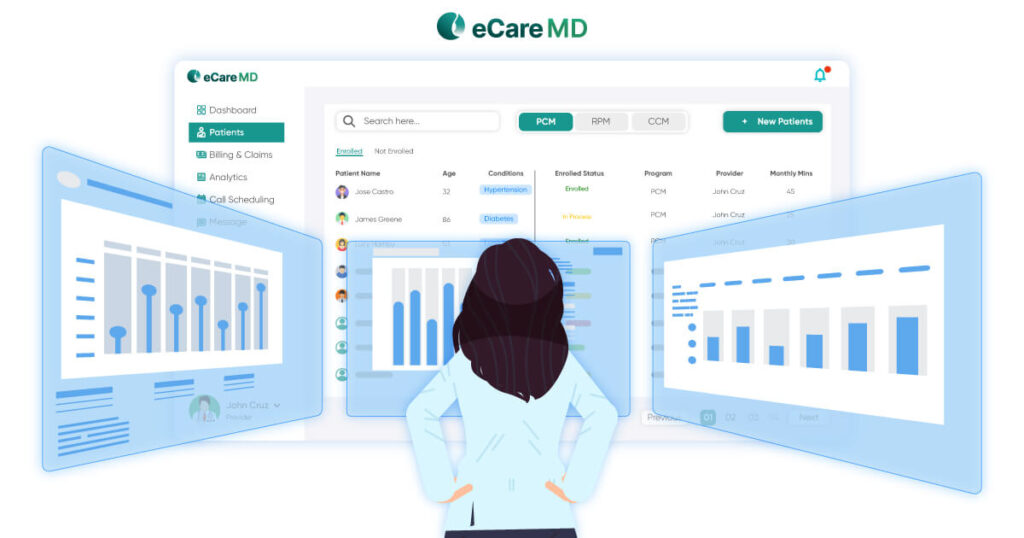
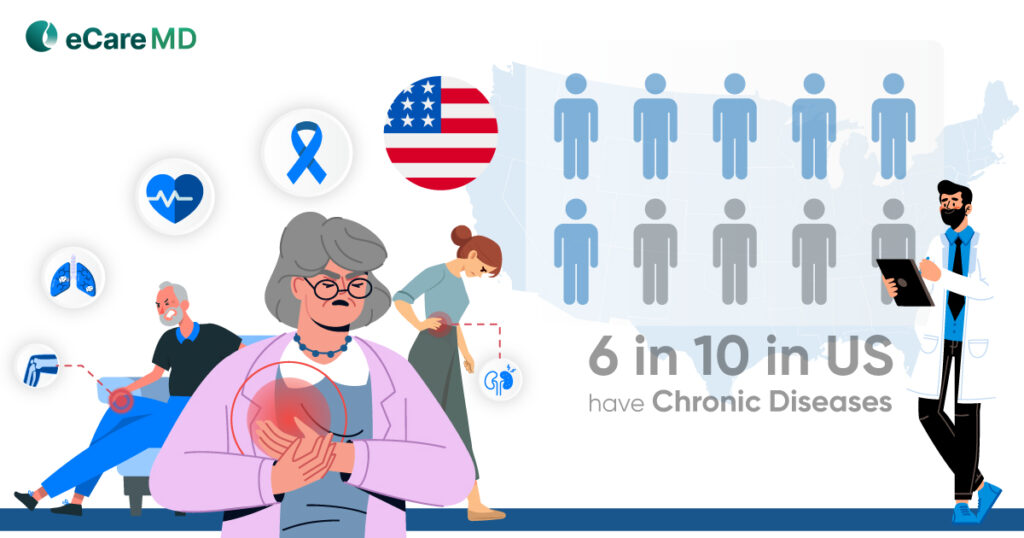
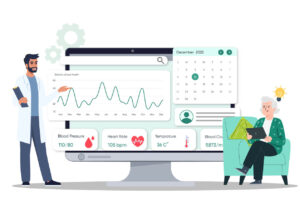
Care coordination software is a platform to manage patients with multiple chronic diseases. Those patients need precise and continuous care. Care coordination software can streamline and improve the quality of care provided by healthcare providers, enabling seamless communication, collaboration, and accessing patient medical records to make an informed decision. Care coordination software has a set of features, such as patient electronic medical record management, appointment scheduling, task management, and telehealth capabilities, including texting and video calling, that can improve patient outcomes.
Care coordination software works keeping the patient medical records at center enabling the real time patient communication along with care team members , automating administrative tasks and insights to make informed decisions to provide a better patient outcome.
The cost of care coordination software can vary widely depending on factors such as the features supported, the size of the practice, the number of users, and vendors’ credibility. Typically, pricing strategies with multiple models, such as one-time fixed cost with some AMC charges, monthly or yearly subscription-based or per patient or per user. These packages have some fixed set of features and functionalities and may have some add-on charges for any customization required, interoperability, and third-party charges.
Additionally, ongoing support and maintenance fees may be included in the total cost. It’s important for healthcare organizations to carefully evaluate pricing options and consider factors such as scalability, support, and return on investment when selecting a care coordination software solution.
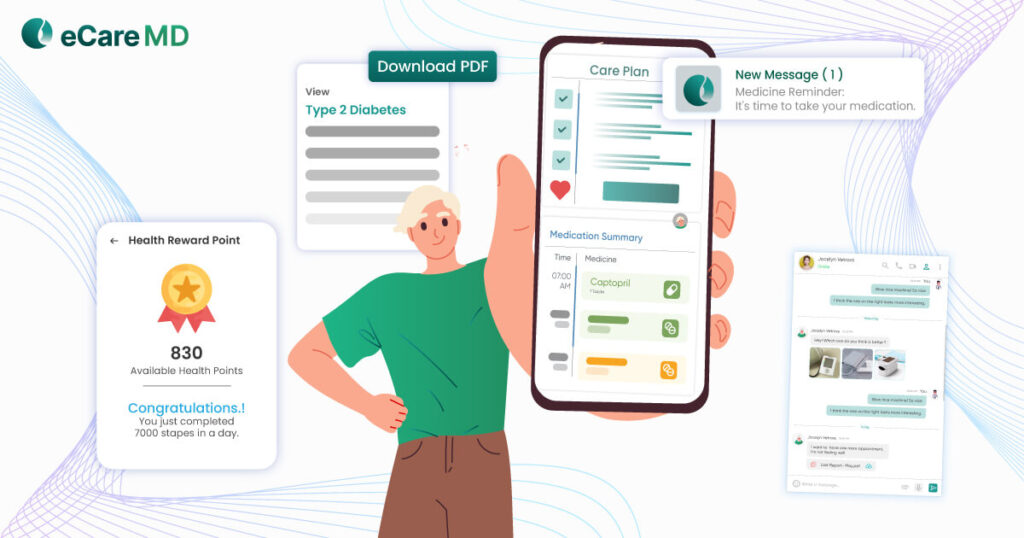
Care coordination software has multiple benefits for all departments within the healthcare organization. For the clinical departments, it streamlines the communication and collaboration between healthcare providers, leads to better care management, reduces manual errors, and improves patient outcomes.
Administrative departments benefit from increased efficiency in tasks such as appointment scheduling, patient data management, and billing, resulting in cost savings and streamlined workflows.
In addition to that, care coordination software improves patient engagement by facilitating communication and care plan sharing, empowering patients to take an active role in their healthcare journey.