Did you face the same kind of challenges in your healthcare platform at your practice to manage your patients smoothly?
What is care coordination software, and how does it work?
5 Ways of Care Coordination Software to Improve Patient Outcomes
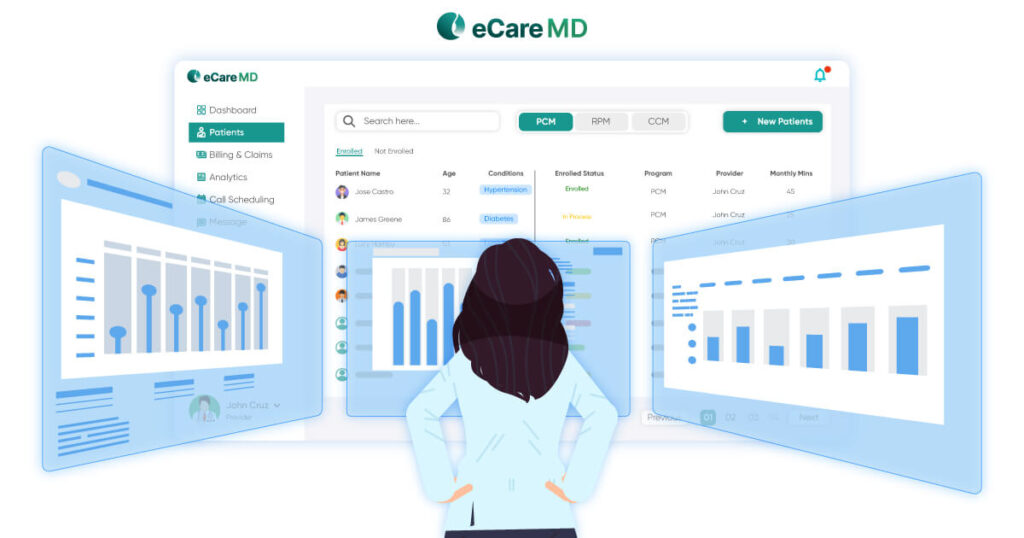
1. Enhanced communication and collaboration
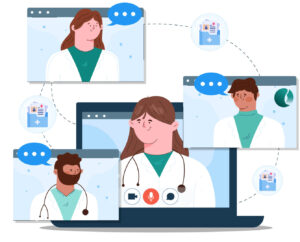 Care coordination software encourages seamless patient communication and collaboration between healthcare teams, including physicians, nurses, specialists, and support staff, using various tools and technology. It enables providers to securely share patient information, facilitating real-time management of care plans, and required interventions. This features in care coordination software streamlines the practice workflows, improving decision making, and ultimately enhancing the quality of care delivered to patient. By leveraging the expertise of multiple healthcare providers, collaboration leads to more holistic and effective patient care.
Care coordination software encourages seamless patient communication and collaboration between healthcare teams, including physicians, nurses, specialists, and support staff, using various tools and technology. It enables providers to securely share patient information, facilitating real-time management of care plans, and required interventions. This features in care coordination software streamlines the practice workflows, improving decision making, and ultimately enhancing the quality of care delivered to patient. By leveraging the expertise of multiple healthcare providers, collaboration leads to more holistic and effective patient care.
2. Improved Care Plan Management
 Care plan creation and management are the keys of care coordination software. It can be improved by centralizing information, allowing caregivers to create and assign care plans seamlessly. Based on a decided routine, the care plan can be updated by getting the patient’s health status. Regular communication and collaboration between the care teams and patients ensure the patient will get quality healthcare services.
Care plan creation and management are the keys of care coordination software. It can be improved by centralizing information, allowing caregivers to create and assign care plans seamlessly. Based on a decided routine, the care plan can be updated by getting the patient’s health status. Regular communication and collaboration between the care teams and patients ensure the patient will get quality healthcare services.
Furthermore, modifying the care plans by identifying the patients tailored need to meet patients health goals and unique needs.Integrating with any Electronic Health Record (EHR) software making sure the patient data is at the right place in a secure environment.This integration reduces the manual data entry efforts along with automated reporting making it easier to bill each service accurately.
3. Streamlined Workflow and Efficiency
 To improve overall productivity and overall resource utilization, optimizing processes and reducing unnecessary steps or delays in healthcare services is required, which can be done by streamlining the workflow and efficiency. This includes identifying the barriers and inefficiencies in practice workflows and implementing strategies to mitigate them. To eliminate this, care coordination software plays a crucial role in streamlining workflows by providing centralized platforms for communication, task management, and data sharing among healthcare team members.
To improve overall productivity and overall resource utilization, optimizing processes and reducing unnecessary steps or delays in healthcare services is required, which can be done by streamlining the workflow and efficiency. This includes identifying the barriers and inefficiencies in practice workflows and implementing strategies to mitigate them. To eliminate this, care coordination software plays a crucial role in streamlining workflows by providing centralized platforms for communication, task management, and data sharing among healthcare team members.
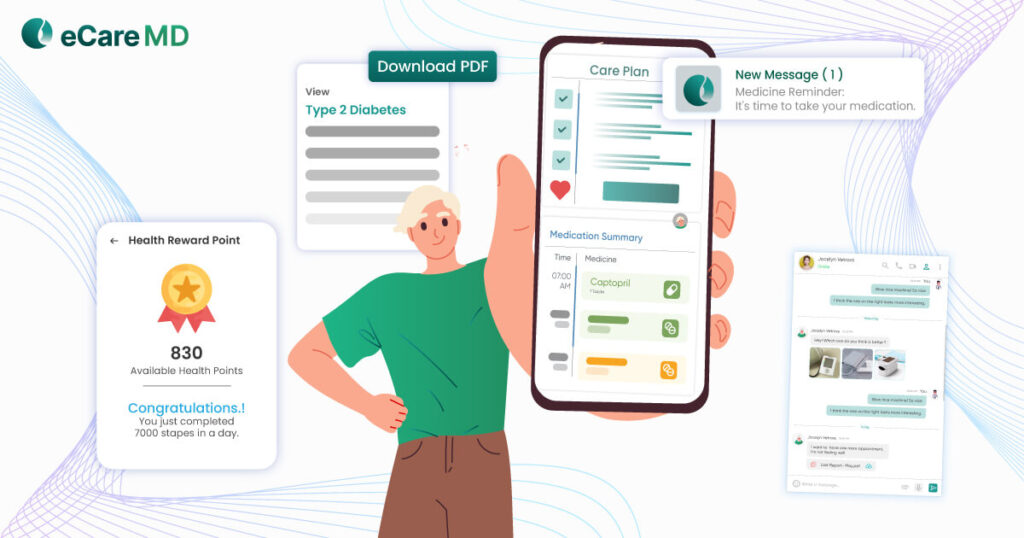
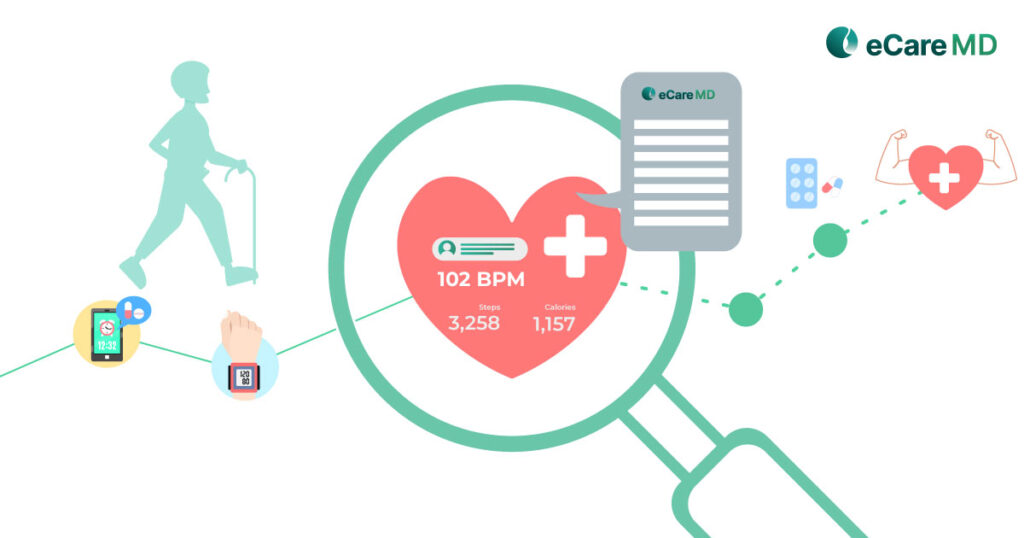
4. Improved Patient Engagement
 Care coordination platforms play a major role in encouraging patients to participate actively in their healthcare journey by enabling them to access their real-time electronic health data. Care coordination platforms have mobile applications that allow patients to access their medical records, lab test reports, care plans, and other information associated with their health. Furthermore, most care coordination platforms have educational resources that can help practices educate patients virtually by sending those through text or email. By promoting health literacy and self-efficacy, these features encourage patients to take a proactive role in managing their health.
Care coordination platforms play a major role in encouraging patients to participate actively in their healthcare journey by enabling them to access their real-time electronic health data. Care coordination platforms have mobile applications that allow patients to access their medical records, lab test reports, care plans, and other information associated with their health. Furthermore, most care coordination platforms have educational resources that can help practices educate patients virtually by sending those through text or email. By promoting health literacy and self-efficacy, these features encourage patients to take a proactive role in managing their health.
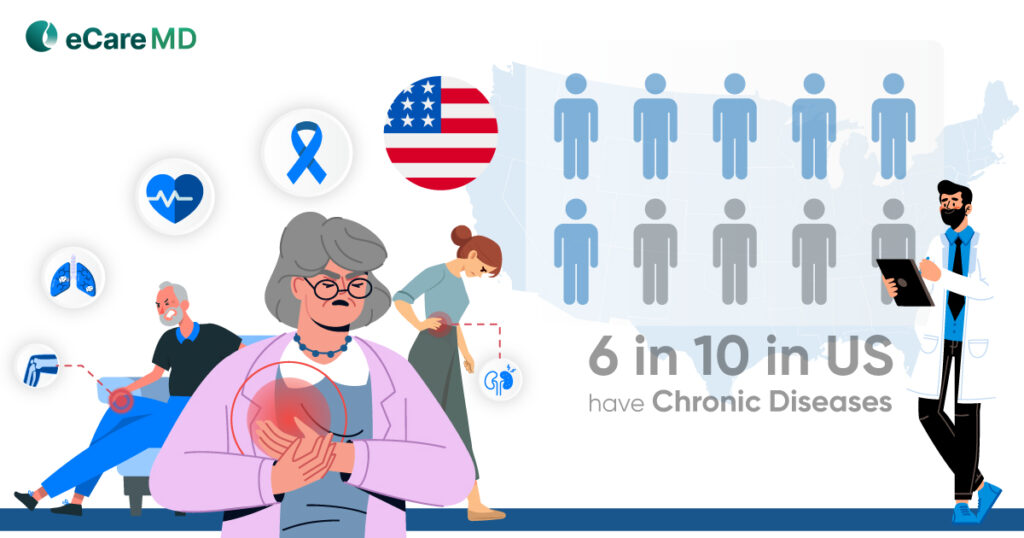
5. Reduced Readmission Rates and Improved Cost Management
 Proper care coordination is the key to prevent hospital readmissions by facilitating seamless transitions between different care settings.By improving the quality of care , care coordination platform determines the gap between the care such as medication management, irregular follow ups,un compliant to the care plan provided which may cause patients get at high risk of complications and get readmitted into the hospitals.
Proper care coordination is the key to prevent hospital readmissions by facilitating seamless transitions between different care settings.By improving the quality of care , care coordination platform determines the gap between the care such as medication management, irregular follow ups,un compliant to the care plan provided which may cause patients get at high risk of complications and get readmitted into the hospitals.
Conclusion
A care coordination platform offers numerous benefits to patients. Patients can actively participate in their health by accessing their medical records, treatment plans, and educational resources. By better understanding and self-management of their health, patients experience improved health outcomes and a higher quality of life.
On the other hand, healthcare providers can improve communication and collaboration between patients and healthcare staff, ensuring everyone involved in patient healthcare is on the same page to deliver quality care. Furthermore, care coordination software can improve resource utilization, which can directly reduce practice management expenses and increase the productivity of healthcare staff.
Frequently Asked Question’s
Care coordination software is a digital tool designed to make seamless communication and collaboration between healthcare providers involved in patient healthcare, as compared to electronic health records (EHRs) or electronic medical records (EMRs), which are made to store and manage patients’ health record within a practices, care coordination software enables patient health information accessible to all associated healthcare providers and patients.
It facilitated multiple ways of patient engagement, going beyond mere data storage by offering features such as secure messaging, care plan management, and task assignment, enabling seamless coordination of care across different healthcare facilities and disciplines. Essentially, care coordination software enhances communication, promotes collaboration, and improves continuity of care by connecting various stakeholders involved in a patient’s health journey.
Care coordination software streamlines the communication between healthcare providers using features such as secure messaging, real-time information exchange, and comprehensive care planning. Task management and tracking of patient care plans help providers monitor patient progress effectively. Additionally, integrating the CCO platform into any EHR or any other system enables healthcare providers to share patient health information securely. Also, while using any EHR, providers can utilize the telehealth capabilities of the CCO platform to achieve better patient engagement and outcomes.
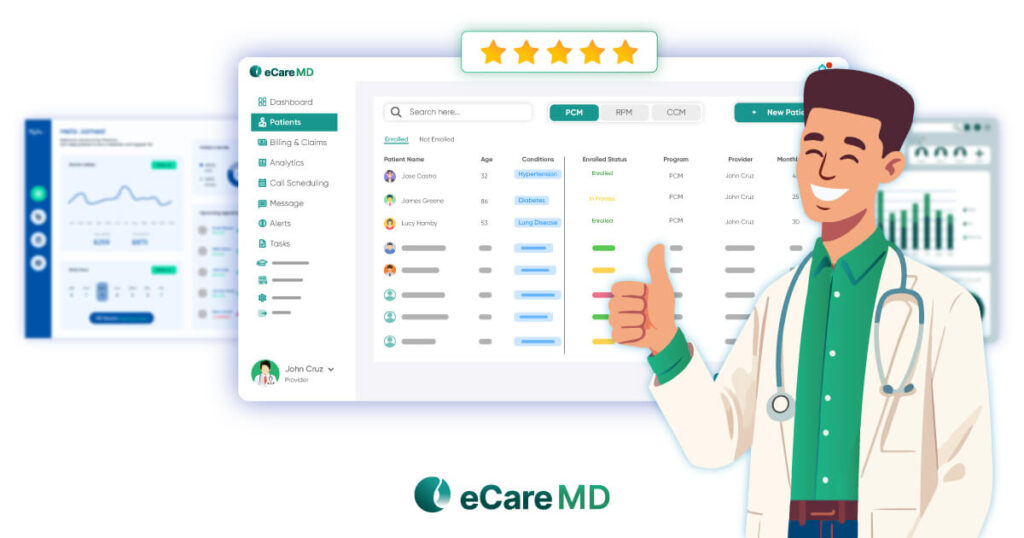
While selecting a care coordination software solution, below are some major features that should be considered for better patient outcomes:
- Secure messaging for communication among healthcare providers.
- Real-time information-sharing capabilities.
- Collaborative care planning tools.
- Task assignment and tracking features.
- Interoperability with electronic health records (EHRs) and other systems.
- Telehealth capabilities for virtual consultations.
- Comprehensive patient data integration.
- Customizable workflows to suit organizational needs.
- Patient engagement tools for active involvement in care.
- Reporting and analytics functionality for performance monitoring.
Implementing the care coordination software is the crucial phase where it has many challenges such as training to staff, interoperability with an existing EHR/EMR system, data privacy and security concerns.
To overcome those challenges, it is important to get each stakeholder involved early in the software implementation process and train them. Interoperability challenge can be addressed by selecting the software which has the ability to easily integrate with any EHR or HIE system to seamless exchange of health information.
Data privacy concerns can be addressed by implementing robust security measures and complying with relevant regulations such as HIPAA. Additionally, ongoing support and feedback mechanisms should be established to address any issues that arise post-implementation, ensuring a smooth transition and successful adoption of the care coordination software.
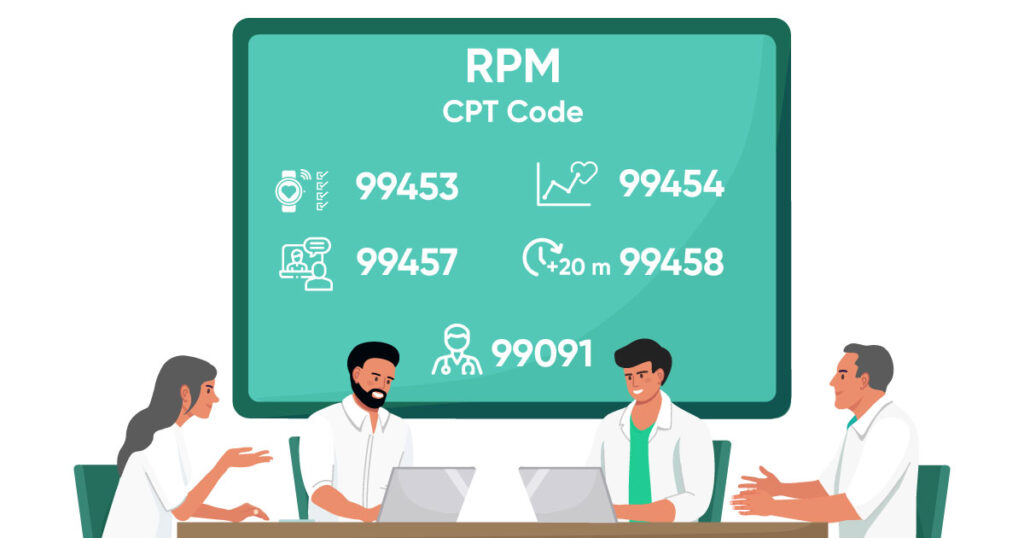
There are various types of care coordination software available on the market, each with its own specific features and capabilities. Below are some examples of care coordination software.
1-Electronic health records.
2-Chronic care management platform
3-Telehealth or telemedicine platform platform
4-Health information exchange software
5-Patient population and engagement platform
Organizations current healthcare workflows, IT infrastructure and readiness of staff are key to ensuring readiness for implementing care coordination software.
Evaluating the existing systems for interoperability and compatibility with the chosen software solution. Proper implementation plan that includes all the go live goals, timelines and responsibilities.Finally, monitor progress closely and gather feedback from users to address any issues and ensure successful adoption of the care coordination software.
Yes, similar to every healthcare software care coordination software is more secure and HIPAA compliant.