Client Overview
The client is a multi-specialty patient management group handling over 600 patients with chronic conditions, from which many have been taken care of by multiple specialist providers, such as cardiologists and primary care physicians. The client practice seeks to manage a smooth workflow to handle patients’ different chronic conditions with an integrated solution platform. The current workflow of care delivery is unstructured with poor care coordination between departments, leading to gaps in care and a communication system.
Business Challenges
1. Unstructured Communication Between Providers
The patient's health update, such as medication changes, hospital follow-ups, and health reports, was not fully shared across care teams, resulting in poor health testing and creating conflict between care teams. Unstructured communication lacks the opportunity to trigger the patient’s critical condition with transparent care.
2. Delayed Interventions Due to Lack of Central Visibility
Providers lacked access to real-time data on patients’ health status, such as patient-centric care plans, Objective vital data, causing delays in response to critical vitals, increasing symptoms, or medication mismanagement.
3. Multi-Point Solutions Without Integration
The practice group used separate systems for patient monitoring, messaging, and follow-up tracking of these procedures do not communicate with the care team, increasing administrative burden. Additionally, tracking care delivery time has also often been missed due to different platforms.

4. Overwhelmed Staff and Missed Follow-Ups
The care team spent excessive time tracking down patient information across their system, which led to missed follow-ups, ignored symptoms, and patient dissatisfaction. The unstructured subjective document has no central management
Solution
The client practice has interacted with Medarch Inc for an integrated platform of care coordination, where Medarch’s team had several interactions with the client to understand the client's business process. After several transparent conversations between both parties, the care coordination software, eCareMD, was introduced, which has seamless care management workflows for patient and provider management. The eCareMD provides centralized visibility within the care team for patient management. Some of the key solutions were implemented as follows;
Solution Highlighted
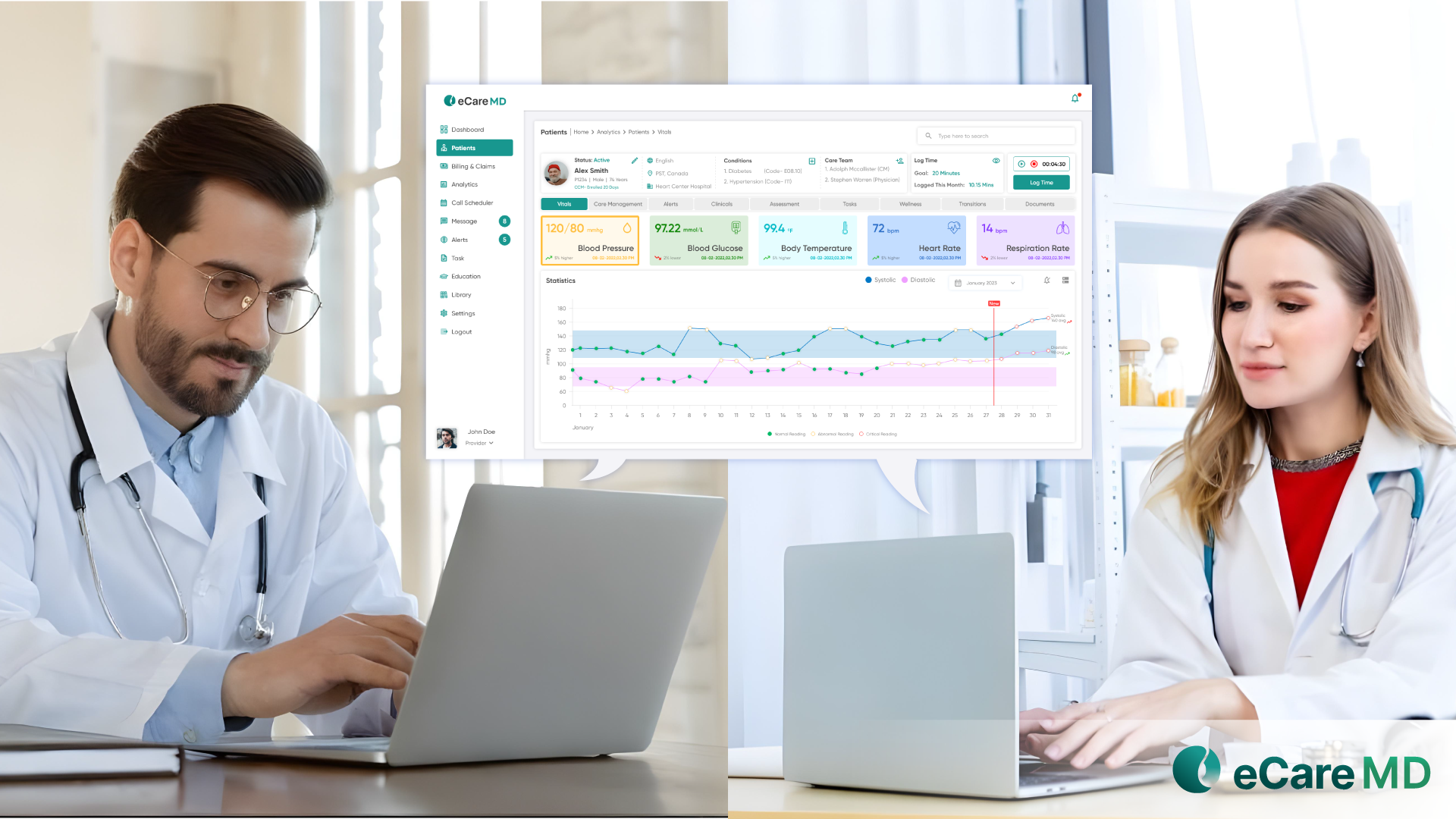
1. Unified Patient Dashboard with Shared Access
All care team members, including physicians, nurses, care managers, and other specialists, gained access to a centralized dashboard that showed patient-centric data and helped to target areas like medication adherence, alerts, and clinical notes, ensuring everyone stayed aligned on patient status. The eCareMD enables role-based access for physicians, nurses, and care managers.
2. AI-Powered Care Coordination Assistant
The AI-enabled eCareMD software provides patients’ data within care programs and marks missing care coordination in areas such as missing care plan, lab results, conflicting medications, and duplication of any information. It recommended robust actions on follow-up calls, referring to primary care, and helping to ensure patients’ safe care.
3. Integrated Secure Messaging and Notifications
The provider team is able to message each other within the eCareMD platform using a seamless communication system with provider-specific task assignment functionality, reducing delays in communication and improving decision-making across departments.
4. Care Plan Documentation and Updates in Real-Time
In the ecareMD platform, providers can view and update personalized condition-oriented care plans collaboratively, and are able to view timely updates by other providers. These care plans can be documented by generating a comprehensive report.
Value Delivered
1. 65% Reduction in Missed Follow-Ups
Automated workflows and visibility into task status helped ensure timely patient engagement, reducing overlooked issues and improving patient trust.
2. Improved Clinical Collaboration Across Departments
Real-time shared access to patients’ data provides better-informed decisions, reduced care conflicts, and faster response to patient needs.
3. Increased Operational Efficiency
By seamless communication and monitoring on a single platform, the administrative workload was reduced by 40%, allowing staff to focus on direct patient care. This results in a 60% increase in operational efficiency.
4. Enhanced Patient Experience and Outcomes
Patients received more comprehensive and proactive care, with fewer gaps, faster interventions, and stronger provider coordination, resulting in impactful improvements in health outcomes and satisfaction.

