Client Overview
The client is a rehabilitation facility network supporting over 500 patients discharged from hospitals after surgeries, strokes, and accidental injuries. These patients were discharged into home-based rehab care, requiring multiple providers such as physical therapists, primary care physicians, and nurses. The facility currently struggles with continuous monitoring of post-discharged patients and increased demand for remote patient monitoring.
Business Challenges
1. Care Fragmentation Post-Discharge
After the patient is discharged and transferred to home care, the care is provided by multiple providers, such as primary care and therapists, who become separated, resulting in lower-level tasks and repeated assessments. The facility is unable to provide different care team specialists within patients' home care, resulting in delays in care delivery.

2. Inconsistent Functional Progress Tracking
The physicians and therapists lacked shared visibility into patient-reported pain and daily health progress, making it difficult to measure progress or adjust care plan productivity. Additionally, patients were in home care, which needed constant monitoring over daily health changes; the care team was unable to track these important changes.
2. Lack of Real-Time Feedback from Patients at Home
The care team is dependent upon patients' health reports, scheduled visits, and follow-ups. Missing these critical real-time data, such as medication adherence, diet plans, and the patient’s routine, will make it difficult to track the patient’s health. At the patient’s home location, the providers failed to provide quality care.
3. Manual Follow-Ups Overwhelming Care Coordinators
The manual process of patient tracking often includes using spreadsheets and phone calls, leading to information errors, duplication of work, and missed follow-ups. Lacking automated workflows for patients’ health tracking makes it difficult for care coordinators.
Solution
To establish a continuous patient monitor, the client had interaction with Medarch Inc., which has robust healthcare products such as care management software eCareMD. Our Business analyst team has several interactive sessions with the client to understand and highlight key business challenges, resulting in the team concluding the areas that need to be automated, where the client’s team has been using manual tools such as Spreadsheets, emails, and log reports.
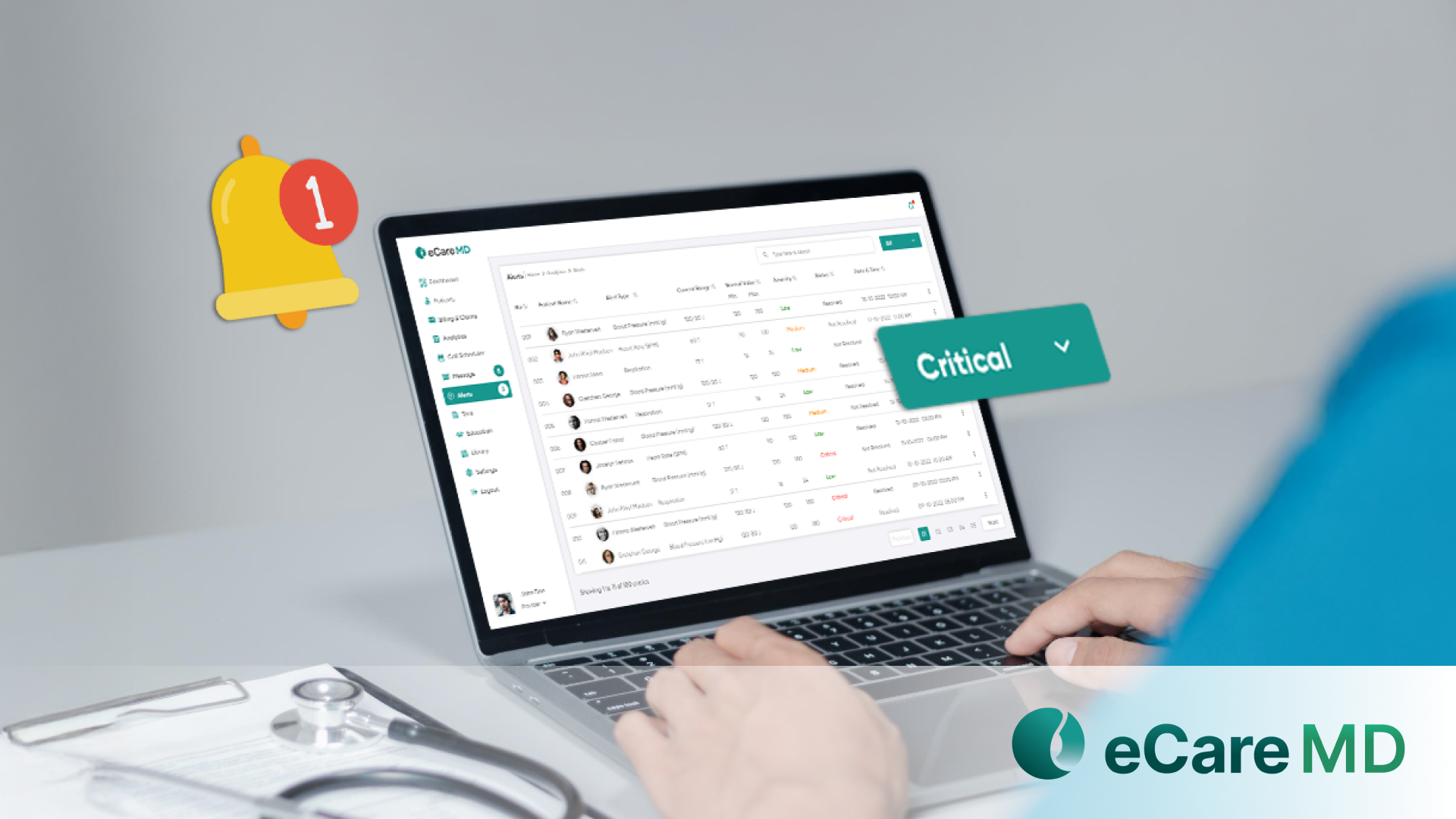
By providing a live demonstration of eCareMD’s robust features like two-way multi-channel communication, progress tracking, and a dynamic program-oriented dashboard, the client partnered with Medarch’s team, where eCareMD has been implemented to resolve these business flows. Some of the key solutions were implemented as follows;
Solution Highlighted
1. Functional Recovery Dashboards
eCareMD enables device integration, where patients are provided with wearable devices that track their movements, such as step count, activity level, and sleep pattern, which are directly shared with physical therapists and physicians. The patients’ progress was measured against their goals with a visualized patient-specific dashboard, and providers predicted the patients’ health outcome and tackled the unwanted insurability with timely interventions.
2. AI-Powered Functional Recovery Predictor
The AI-powered functional recovery predictor of eCareMD analyzes rehab trends such as daily activity level, adherence to therapy tasks, etc., and predicts the possibility of recovery completion within a pre-defined time duration. It flagged patients based on their recovery level and suggested interventions like timely follow-ups, medication reconciliation, and providing education to the patients. It also provides auto suggestions to the patient regarding taking their daily vitals, medications, and following the routine.
3. Fall Risk & Recovery Alert System
eCareMD provides the feasibility where providers can configure abnormal vitals/ activities such as disturbed sleep, missed exercise, or inconsistency in vital readings according to the patient’s health risk to notify coordinators and therapists for immediate interventions, helping the care team to get notified early to provide necessary action. The alert system also supports different media such as Text/SMS, Emails, and push notifications to deliver alert messages on time.
4. Shared Progress Notes & Treatment Adjustments
The care team members,l ike therapists and nurses, shared the updated care plans, notes in real-time based on the patient’s observations, vitals, and feedback, ensuring every care member had access to the latest patient’s health status without needing multiple assessments. This helped the practice provide the required multidisciplinary care to the patients.
Value Delivered
1. 50% Reduction in Missed Therapy Appointments
With role-based access, which allows care team members to share coordination and automated follow-up workflows, the client’s practice saw a significant improvement in appointments, decreasing no-shows and delays in treatment milestones.
2. Improved Rehab Goal Achievement Rates by 42%
The patients monitored with eCareMD’s RPM features achieved their progress goals successfully faster due to early alert and interventions on patients' health decline.
3. Reduced Burden on Care Coordinators by 60%
Automated tracking, notifications, and shared communication logs replaced manual outreach and scheduling spreadsheets.
4. Stronger Multidisciplinary Collaboration
For the first time, therapists, physicians, nurses, and coordinators operated from the same interface with real-time data, reducing duplication and enhancing care quality.

