Client Overview
The client has a multi-specialty group in Georgia, USA, serving a diverse patient population across endocrinology, pulmonology, and nephrology, with the goal of implementing Medicare's Principal Care Management (PCM) to deliver structured, reimbursable care to patients with chronic conditions. The primary goal is to successfully achieve PCM enrollment while maintaining seamless clinical workflows.
Business Challenges
While serving diverse patients and planning to start PCM care management services, the client has researched the business-oriented requirements, where they find out some of the key challenges that need to be addressed before delivering PCM care services as follows:
1. Inconsistent eligibility screening:
While conducting bulk patient outreach for the client business, it is hard to check the program eligibility of patients. When managing diverse patients across different specialties, the predefined PCM program eligibility is essential for bulk enrollment. This inconsistency in eligibility screening is causing a significant time-consuming process, delaying enrollment of patients in the program and starting to provide care.
2. Delayed Consent collection:
In order to bill PCM services, the provider must obtain the patient's consent to provide PCM services. Currently, the client's business has failed to maintain structured consent and faces delays in collection. These results show that patients who are eligible for PCM may not be enrolled on time, reducing the enrollment scale of the RPM program.
3. Unstructured care plan progression tracking:
Inconsistencies in care plan progress tracking can delay patients' clinical follow-ups, where the care team can not consistently monitor the patient's health at each level, like whether their health is improving, regressing, or needs interventions. This lack of visibility affects patient outcomes and makes PCM billing difficult to justify.
4. Documentation gap in Non-face-to-face Services:
The required documentation in non-face-to-face activities, such as phone calls, care plan reviews, symptoms, and patient education, results in a loss of opportunity for both clinical and reimbursement processes. While the interactions are not consistently recorded, the care team fails to oversee patient interventions.

Solution provided
The Client provider team, while suffering from several business challenges, in order to tackle these situations, reached out Medarch team for care coordination software, where they interact with Medarch’s eCareMD Care Coordination Software. The solutions were implemented to tackle the client’s ongoing business challenges in PCM care management. The key solution was implemented as below:
Solution Highlighted
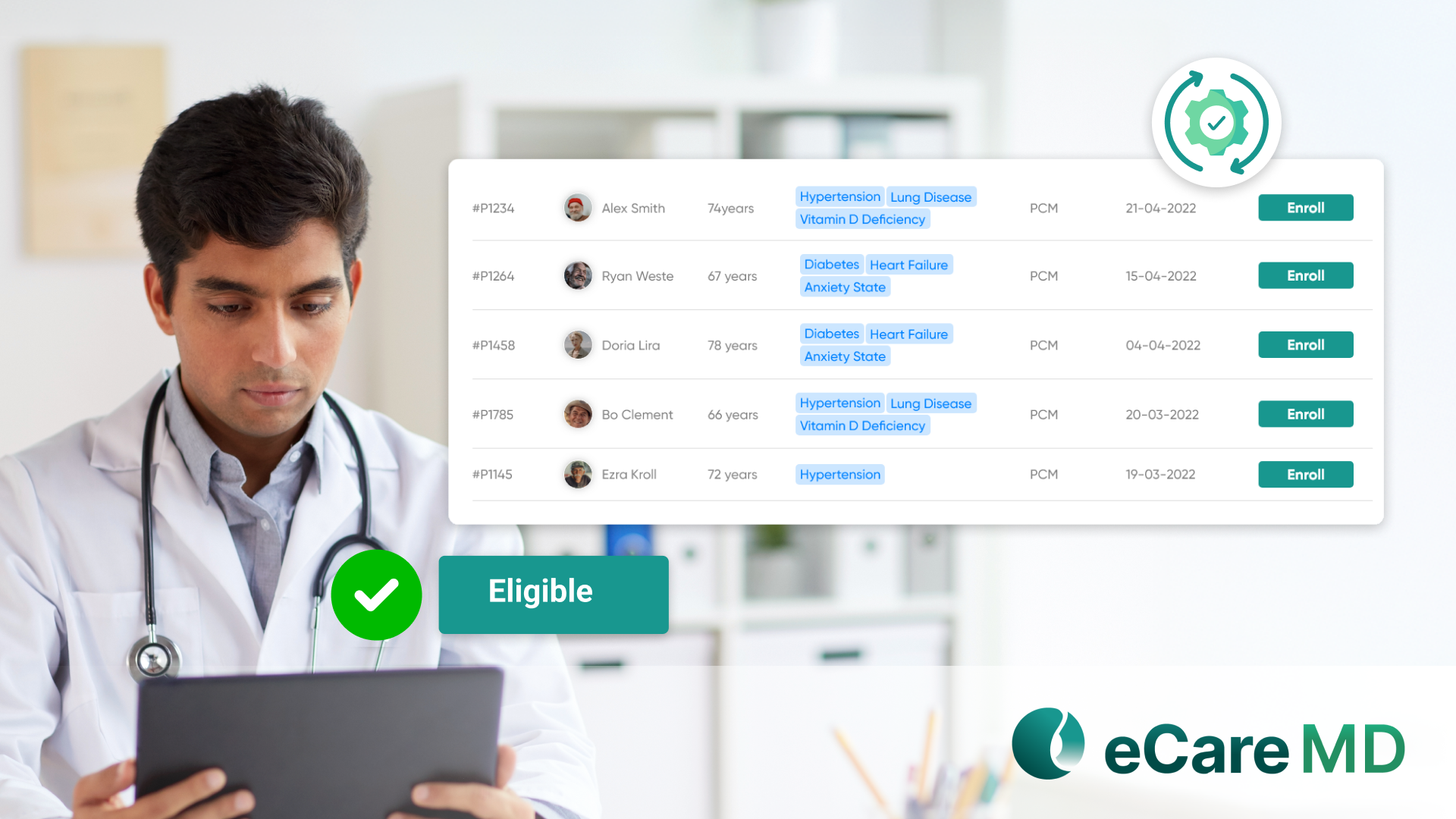
1. Automated Eligibility Engine:
While understanding the importance of pre-defined eligibility for program enrollment, the “eCareMD” software automatically detects patient eligibility for a PCM Program based on chronic conditions. By which provider do patients enroll directly into the PCM program? This saves providers time on manual detection of program eligibility.
2. Flexible Consent Workflow:
The consent obtaining is a crucial part before starting PCM care management. The eCareMD provides a seamless workflow to obtain consent, based on CMS compliance, which gives providers that the ability to obtain consent verbally, digitally, and in writing to enroll patients into the program.
3. Care Plan Assignment Tools:
The platform has a dedicated care plan management module to track patient care progress, from which providers can assign a care plan, track their symptoms, goals, interventions, and timely updates. These tools help to maintain patients’ health and are used to trace every activity related to patients. This is the key process to get the PCM code qualified.
4. Auto Time Tracking for Virtual Interaction:
For non-face-to-face interactions, the eCareMD has auto time tracking functionality for activities such as phone calls, email, care plan review, etc. Additionally, it documents all these logs into the respective patient chart and adds these logs for billing purposes. These accurate log reports justify the billable codes, helping the client in the reimbursement process.
Value Added to the client practice
1. Successfully Enrolled 700+ in 90 Days:
The eCareMD’s seamless patient onboarding process is managing the bulk enrollment process with an auto program eligibility system and bulk patient outreach. This impact on the client's business is to add 700+ patients in the PCM program over 90 days, which is considered a big revenue success.
2. Medicare PCM Revenue with a 98% Claim Success Rate:
The proper documentation for each clinical and reimbursement process has boosted reports, helping clients to get 98% of claims success in PCM care management.
3. Strengthened Clinical Outcomes Through Proactive Monitoring:
The CareMD has a single platform to manage patient-oriented clinical activities, resulting in proactive monitoring to obtain patient health outcomes.
4. Higher Satisfaction in Patients due to Feeling Supported and Monitored Between Visits:
The non-face-to-face functionalities of eCareMD provide significant patient engagement over patient monitoring, resulting in higher satisfaction in patients due to feeling supported and monitored.

