Client Background
A healthcare provider based in Alaska has gained popularity for their passion, medical expertise, and willingness to deliver care services to patients suffering from chronic diseases. The client manages patients through their traditional healthcare practice and uses chronic care management software to deliver care to the patients.
Business challenges
Some of the business challenges faced by the client while managing patients are:
1. Challenges in importing patients through EHR
To obtain maximum reimbursement, it is important to enroll as many patients as possible. This will be possible only if the provider has a sufficient number of patients willing to enroll in the program. The client’s CCM software does not offer the functionality to directly import the CSV/CCDA file imported from the different EHR software and upload it to the existing platform. This lack of functionality resulted in the loss of opportunities of enrolling as many patients as the client won’t be able to reach a maximum number of patients and get them enrolled.
2. Challenges in patient eligibility tracking
Identification of eligible patients for enrollment in the program is a crucial aspect of practices. Despite multiple patients available in the software, the client’s platform lacked the functionality to identify eligible patients for the CCM program. This hampered delays in getting patients enrolled in the program, resulting in the loss of reimbursement.
3. Difficulties in patient outreach
The initial step in enrolling patients in the program involves reaching out to them and informing them about the benefits of enrollment. Unfortunately, the client's existing CCM software lacks the capability to communicate with patients prior to enrollment. As a result, the client faced challenges in reaching a larger number of patients and enrolling them in the program, leading to revenue loss.
4. Patient’s unawareness of the benefits of enrollment in the program
One of the significant challenges the client has faced is the patients are unaware of the benefits of getting enrolled in the program. Hence, they won't show their willingness to participate in the program. The client wasn’t able to address this challenge, which hampered the enrolled patient count and ultimately reduced the reimbursement amount from the insurance company.
Solution
To figure out the client’s business challenges and exact requirements, our team has coordinated with the client over calls and shown demonstrations of how eCareMD CCM software will resolve the challenges. After receiving approval from the client, our team has implemented the eCareMD software into the client’s practice, and the client has experienced significant growth in patient enrollment.
Solution Highlights
Some of the best features that overcame the client’s business challenges and increased the enrolled patient count are:
1. CSV/CCDA File import
It is important that the provider has a large number of patients to increase the number of enrolled patients. The eCareMD software has resolved this issue, as it integrates with the EHR software and pulls all patients from the EHR software into the platform. Also, if the user has a CSV/CCDA file handy, then eCareMD allows them to upload it within the platform, which helps to create hundreds of patients with a single click. This functionality helped significantly in increasing the enrolled patient count.
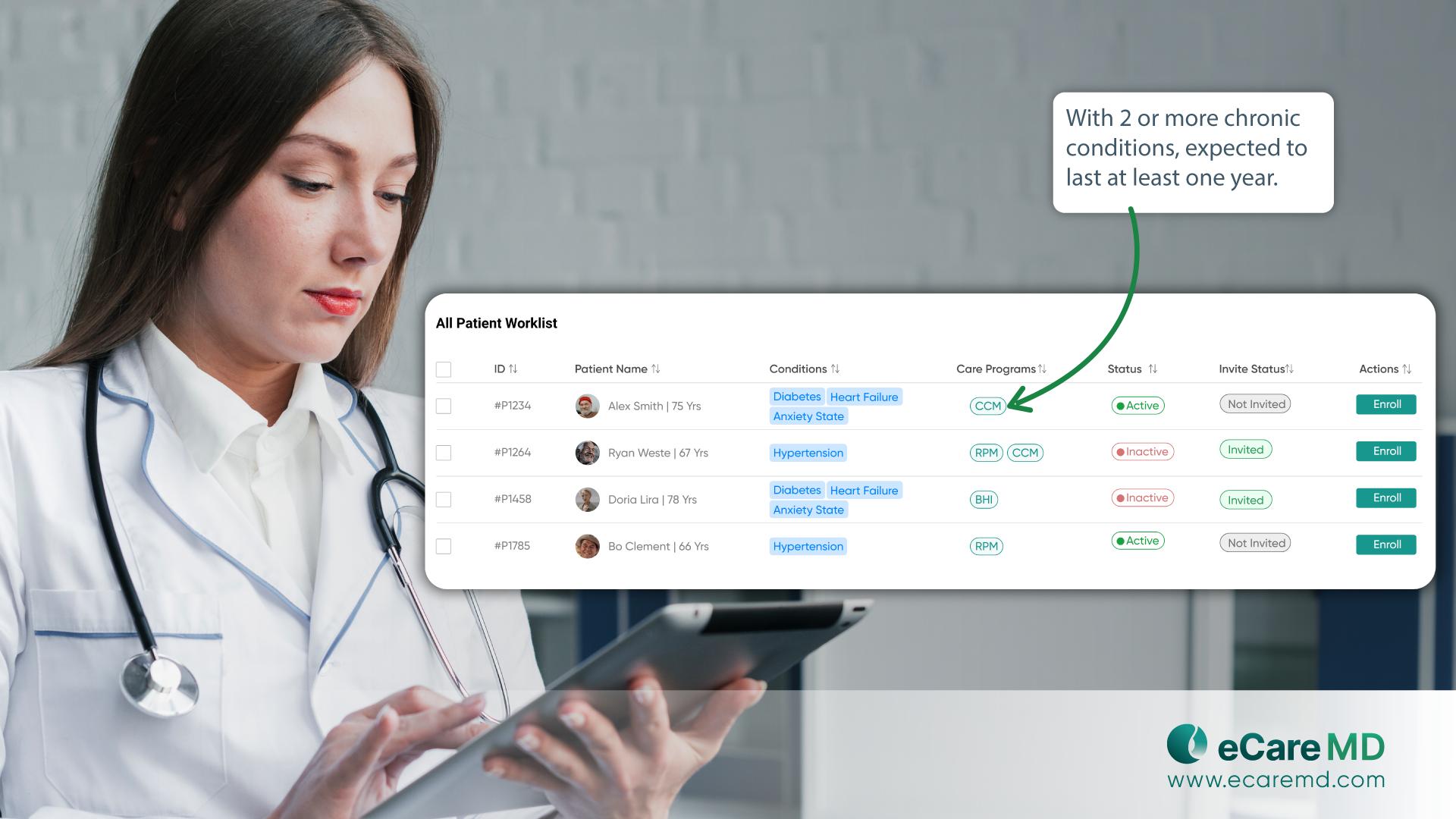
2. Automated patient eligibility tracking
The eCareMD software has made it simple for care providers to identify eligible patients and enroll them in the CCM program. The software is built with logic that recognizes the number of chronic conditions the patient has and the duration of their suffering from that chronic disease. Based on the patient details, the software marks the patient as eligible for various programs, which helps care providers quickly identify eligible patients and enroll them in the CMS-sponsored program.
3. Bidirectional communication functionality
Interaction with patients and empowering them to enroll in the CMS-sponsored program is a crucial aspect of delivering care. The eCareMD software allows care providers and admin staff to make outcalls and send SMS to patients through the platform. Patients can also reach care providers with any queries or suggestions using the same contact details.
This increase in interaction helped care providers, reach the maximum number of patients and enroll them by empowering them to reap the benefits of participating in the program.
4. Send educational material
It is important that the patient be aware of the benefits they will get in order to obtain patient consent for participation in the program. To improve awareness about program benefits and empower patients about their chronic conditions, the eCareMD software allows care providers to store educational materials within the software and send them to the patient via email or text message.
The client has shared the CMS documentation, which describes the benefits, procedure, eligibility, and treatment plans, and has encouraged patients to participate in the program. Subsequently, the patient enrollment count has been increased.
Value Delivered
1. Rapid Patient Onboarding
Integration with EHR software and the ability to import CSV/CCDA files into eCareMD streamline the patient onboarding process. This functionality allows care providers to quickly add large numbers of patients to the platform, significantly increasing the enrolled patient count.
2. Streamlined Enrollment Process
eCareMD's automated patient eligibility tracking simplifies the identification and enrollment of eligible patients into CCM programs. By automatically assessing patient eligibility based on predefined criteria, care providers can efficiently enroll patients without manual intervention.
3. Enhanced Enrollment Rates by 45%
By maximizing patient-provider communication, eCareMD ensures that care providers can efficiently reach out to a larger number of patients, resulting in 45% higher enrollment rates for CMS-sponsored programs.
4. Informed Patient Consent
eCareMD's capability to send educational materials to patients enhances awareness of program benefits and treatment plans, empowering patients to make informed decisions about participating in CMS-sponsored programs.

