Client Overview
Located in Brooklyn, NY, USA, the client's clinic has an Interventional Cardiology Group with a specialty team in cardiology. Performing 500+ procedures annually. Provider of PCM care coordination services to post-cardiac recovery patients. Ensuring proper collaboration and coordination between patients and providers in the PCM program. To improve post-procedure outcomes, reduce complications, and enhance patient satisfaction scores.
Business Challenges
The client’s current care services are based on traditional ways to treat patients, while providing PCM care, they’re facing major business challenges that are affecting their quality of care. Some of the major business challenges are as below :
1. No digital automated workflows to manage PCM-oriented requirements
The client provider team has been dealing with traditional workflows to manage their day-to-day tasks. Because of the lack of digital automated workflows specifically for PCM-oriented requirements, the manual tasks consume more man-hours on repetitive tasks such as care plan creation, goals tracking, patient engagement, etc. Spending these man-hours on manual tasks results in a vast amount of time loss for the client’s business.
2. Difficulty tracking patients’ Interactions and time logs
The current process of providing PCM care services has no ability to manage patient interactions, as well as to qualify for PCM codes required for logging each time of care delivered. These are the most important areas where the client's business holds back in order to deliver quality care and accurate time log management, resulting in missing delivered care services and a lack of transparency.
3. Challenges in capturing accurate data for CMS’s PCM Reimbursements
For a timely reimbursement process, it is necessary to maintain accuracy in the data that is being used for the reimbursement process. Currently, the client's business has failed to maintain accuracy while generating related information about their caregiving process, resulting in failed claim submission entries, which affect the client's overall revenue.

4. Lack of a standardized care plan specifically for cardiac chronic conditions
As the current process has a structured care plan creation process, it has very little for providers to keep care plans specific to cardiac chronic conditions. As multiple conditions occur, it is required to have care plans in PCM programs where the client has poor care plan management, resulting in compromised care plan quality and difficulty in managing the same.
Solution Provided
As the client has observed, the critical areas where the business is lacking are in delivering care. In order to overcome these challenges, the team has reached out to the Medarch team, where multiple requirement-gathering sessions have been conducted to tackle the business problem and came up with a solution where the Care Coordination Software - erCareMD was put in place to manage clients’ business digitally. Some of the key solutions were implemented as below:
Solution Highlighted
1. Specialty-specific care plan template for cardiac conditions
The eCareMD has a dedicated Library Module, which has over 160+ care plan templates based on each chronic condition. These care plans can be directly assigned to patients, also based on their chronic condition, which automatically fetches, saving valuable time for care team members to assign and update condition-specific care plans.
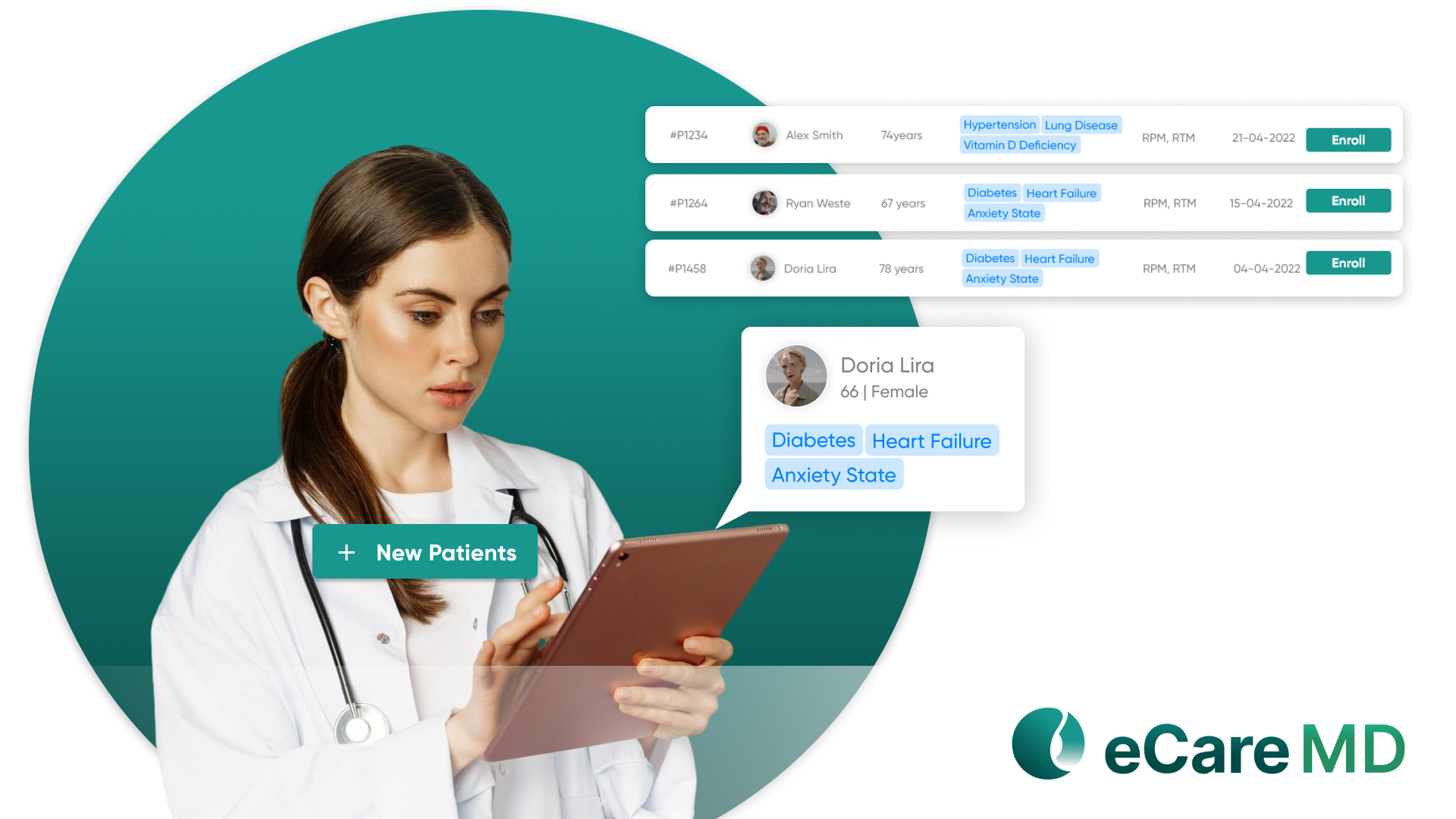
2. Automated patient enrollment workflows with eligibility verification
The implemented “eCareMD” care coordination software has automated patient enrollment workflows from which providers can enroll patients into PCM, CCM, and RPM programs by digital, verbal, and written methods. The platform also detects the program eligibility based on the patient’s conditions.
3. Integrated time tracking for non-face-to-face activities
While delivering PCM services, it is important to qualify CPT codes based on time logging. The eCareMD has an auto-time logging system for each activity performed by the care team member for patients, such as care plan assignment, review, tracking progress updates, vital review, voice calling over the patient, assigning assessments, and tasks. The automated features solve major problems while providing non-face-to-face care services.
4. Reimbursement tracking for billing insights
The eCareMD software automatically generates the qualified CPT code for each patient in the “Billing & Claim” module. The Patients are listed based on time spent by the care team member in billing each month, from which the provider can generate standardized reports for billing, including CPT codes. It module also works by sending these billing reports directly to the biller role on that specific tenant at the end of each month. The report can be saved in PDF format. Along with these, the dashboard shows analytics of billing for that particular month.
Value Delivered
1. Enabled onboarding of 300+ eligible PCM patients within 90 days
The seamless onboarding process of eCareMD enabled the onboarding of 300+ eligible patients within 90 days. The platform marked the eligibility criteria based on the patient’s condition. That amount of enrollment process ensures the PCM reimbursement and boosts client revenue.
2. Empowered care managers to handle 3x more patients with automated support
The bulk patient upload through CVS, Auto program eligibility, and automated report-generating features are providing a boost to provider work, handling 3x more patients on a single portal.
3. Increased monthly PCM revenue by 24% by optimizing billing and care tracking
The optimized billing and clinical reports have helped increase monthly PCM revenue by 24% as the reimbursement rate increased with the quality of reports and audit logs.

